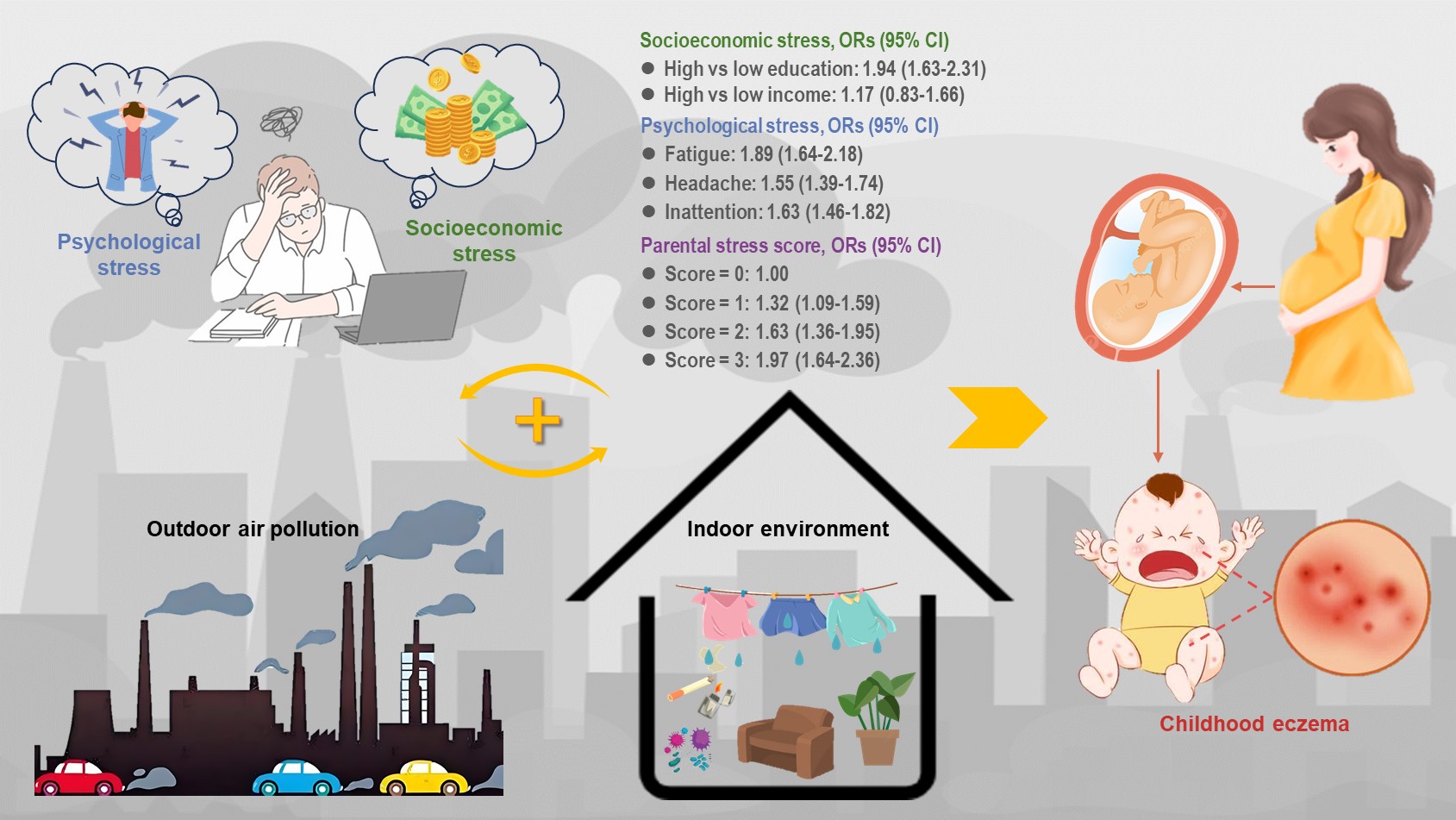
- Parental stresses are associated with children’s physician-diagnosed eczema (PDE)
- High parental socioeconomic stress increased PDE risk of decoration and allergens
- High parental social stress elevated the impact of prenatal exposure to NO2 on PDE
- Parental psychological stress enhanced PDE risk of PM2.5–10 and PM10 exposure
- There is a “stress-environment interaction” on the development of childhood eczema
- Open Access
- Article
Interactions of Parents’ Stress and Environmental Factors on Children’s Eczema: Key Roles in Allergens and Air Pollution
- Chan Lu 1, 2, 3, *, †,
- Yuqing Chen 1, †,
- Junlong Yun 1, †,
- Jing Ma 1,
- Wenying Sun 1,
- Wen Deng 1,
- Xianglong Xiao 1
Author Information
Received: 25 Sep 2025 | Revised: 30 Oct 2025 | Accepted: 04 Nov 2025 | Published: 06 Nov 2025
Highlights
Abstract
Increasing evidence linked air pollution and social stress with eczema independently, yet their interactive effects on childhood eczema in early life are unknown. This study aimed to explore the effects of parental stresses and their interactions with interior and extraventricular environmental exposures on preschooler’s physician-diagnosed eczema (PDE). We conducted a mixed cross-sectional and retrospective cohort study involving 8689 children at Changsha in China. Individual data for health information, parental stresses, and interior environments were collected through questionnaires. Individual exposure to temperatures and extraventricular pollutants were computed using the Inverse Distance Weighted (IDW) technique method. Multivariable logistic regression analyses were engaged in this research. We found that childhood PDE was markedly associated with higher education among parents (ORs [95% CI] = 1.94 [1.63–2.31]), while presence of fatigue, headache and distractibility amplified PDE risk (1.89 [1.64–2.18], 1.55 [1.39–1.74] and 1.63 [1.46–1.82]). Higher score of parental psychological stresses was related to elevated risks of PDE. Parents owning lower education or income had higher childhood PDE risk of moldy clothing/bedclothes, nonflowering plants, decoration throughout pregnancy till previous year. PDE risk from PM2.5, NO2 and O3 exposure mainly before birth were higher in families with high social stress. PDE risk from early life exposure to PM2.5, PM2.5–10, PM10, and NO2 during preconception, first year, and entire postnatal stage was higher in parents with psychological stress. Our study indicates that early life exposures to parental stresses as well as their combinations with interior and outdoor pollution and allergen increased risk of childhood PDE, suggesting the “(pre-)fetal origin of eczema” hypothesis through stress-environment interaction.
Graphical Abstract
Keywords
childhood eczema | parents’ psychological stress | traffic-related air pollution | early life exposure | stress-environment interaction
References
- 1.Ridd, M.J.; Wells, S.; Edwards, L.; et al. Best emollients for eczema (BEE)—comparing four types of emollients in children with eczema: protocol for randomised trial and nested qualitative study. BMJ Open 2019, 9, e033387.
- 2.Beasley, R. Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet 1998, 351, 1225–1232.
- 3.Guo, Y.; Li, P.; Tang, J.; et al. Prevalence of Atopic Dermatitis in Chinese Children aged 1–7 ys. Sci. Rep. 2016, 6, 29751.
- 4.Lu, C.; Norbäck, D.; Zhang, Y.; et al. Onset and remission of eczema at pre-school age in relation to prenatal and postnatal air pollution and home environment across China. Sci. Total Environ. 2021, 755, 142467.
- 5.Lu, C.; Li, Q.; Qiao, Z.; et al. Early and late onset childhood eczema: Role of preconceptional, pre-natal and post-natal environmental exposures. Build. Environ. 2024, 258, 111626.
- 6.Ramírez-Del-Pozo, M.E.; Gómez-Vera, J.; López-Tiro, J. Risk factors associated with the development of atopic march. Case-control study. Rev. Alerg. Mex. 2012, 59, 199–203.
- 7.Chamlin, S.L.; Frieden, I.J.; Williams, M.L.; et al. Effects of atopic dermatitis on young American children and their families. Pediatrics 2004, 114, 607–611.
- 8.Kermack, W.O.; McKendrick, A.G.; McKinlay, P.L. Death-rates in Great Britain and Sweden. Some general regularities and their significance. Int. J. Epidemiol. 2001, 30, 678–683.
- 9.Gluckman, P.D.; Hanson, M.A.; Cooper, C.; et al. Effect of in utero and early-life conditions on adult health and disease. N. Engl. J. Med. 2008, 359, 61–73.
- 10.Bai, J.; Zhao, J.; Shen, K.L.; et al. Current trends of the prevalence of childhood asthma in three Chinese cities: a multicenter epidemiological survey. Biomed Environ. Sci. 2010, 23, 453–457.
- 11.Lee, S.L.; Lau, Y.L.; Wong, H.S.; et al. Prevalence of and Risk Factors for Childhood Asthma, Rhinitis, and Eczema in Hong Kong: Proposal for a Cross-Sectional Survey. JMIR Res. Protoc. 2017, 6, e7252.
- 12.Li, F.; Zhou, Y.; Li, S.; et al. Prevalence and risk factors of childhood allergic diseases in eight metropolitan cities in China: a multicenter study. BMC Public Health 2011, 11, 437.
- 13.Zhang, Y.; Li, B.; Huang, C.; et al. Ten cities cross-sectional questionnaire survey of children asthma and other allergies in China. Chin. Sci. Bull. 2013, 58, 4182–4189.
- 14.Zhao, T.; Wang, H.J.; Chen, Y.; et al. Prevalence of childhood asthma, allergic rhinitis and eczema in Urumqi and Beijing. J. Paediatr. Child. Health 2000, 36, 128–133.
- 15.Shalowitz, M.U.; Mijanovich, T.; Berry, C.A.; et al. Context matters: a community-based study of maternal mental health, life stressors, social support, and children’s asthma. Pediatrics 2006, 117, e940–e948.
- 16.Yamamoto, N.; Nagano, J. Parental stress and the onset and course of childhood asthma. Biopsychosoc. Med. 2015, 9, 7.
- 17.Dohrenwend, B.S. Social status and stressful life events. J. Pers. Soc. Psychol. 1973, 28, 225-235.
- 18.Lewis-Jones, S. Quality of life and childhood atopic dermatitis: the misery of living with childhood eczema. Int. J. Clin. Pract. 2006, 60, 984–992.
- 19.Seeman, T.E.; Crimmins, E.; Huang, M.H.; et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc. Sci. Med. 2004, 58, 1985–1997.
- 20.Miller, G.; Chen, E. Unfavorable socioeconomic conditions in early life presage expression of proinflammatory phenotype in adolescence. Psychosom. Med. 2007, 69, 402–409.
- 21.Kubzansky, L.D.; Kawachi, I.; Sparrow, D. Socioeconomic status, hostility, and risk factor clustering in the Normative Aging Study: any help from the concept of allostatic load? Ann. Behav. Med. 1999, 21, 330–338.
- 22.Silverberg, J.I.; Hanifin, J.M. Adult eczema prevalence and associations with asthma and other health and demographic factors: a US population-based study. J. Allergy. Clin. Immunol. 2013, 132, 1132–1138.
- 23.Arndt, J.; Smith, N.; Tausk, F. Stress and atopic dermatitis. Curr. Allergy Asthma Rep. 2008, 8, 312–317.
- 24.Peters, E.M. Stressed skin?—A molecular psychosomatic update on stress-causes and effects in dermatologic diseases. J. Dtsch. Dermatol. Ges. 2016, 14, 233–252.
- 25.Flanigan, C.; Sheikh, A.; DunnGalvin, A.; et al. Prenatal maternal psychosocial stress and offspring’s asthma and allergic disease: A systematic review and meta-analysis. Clin. Exp. Allergy 2018, 48, 403–414.
- 26.Andersson, N.W.; Hansen, M.V.; Larsen, A.D.; et al. Prenatal maternal stress and atopic diseases in the child: a systematic review of observational human studies. Allergy 2016, 71, 15–26.
- 27.Min, K.D.; Yi, S.J.; Kim, H.C.; et al. Association between exposure to traffic-related air pollution and pediatric allergic diseases based on modeled air pollution concentrations and traffic measures in Seoul, Korea: a comparative analysis. Environ. Health 2020, 19, 6.
- 28.Yi, S.J.; Shon, C.; Min, K.D.; et al. Association between Exposure to Traffic-Related Air Pollution and Prevalence of Allergic Diseases in Children, Seoul, Korea. Biomed. Res. Int. 2017, 2017, 4216107.
- 29.Deng, Q.; Lu, C.; Li, Y.; et al. Exposure to outdoor air pollution during trimesters of pregnancy and childhood asthma, allergic rhinitis, and eczema. Environ. Res. 2016, 150, 119–127.
- 30.Bråbäck, L.; Forsberg, B. Does traffic exhaust contribute to the development of asthma and allergic sensitization in children: findings from recent cohort studies. Environ. Health 2009, 8, 17.
- 31.Liu, W.; Cai, J.; Huang, C.; et al. Associations of gestational and early life exposures to ambient air pollution with childhood atopic eczema in Shanghai, China. Sci. Total Environ. 2016, 572, 34–42.
- 32.Bose, S.; Chiu, Y.M.; Hsu, H.L.; et al. Prenatal Nitrate Exposure and Childhood Asthma. Influence of Maternal Prenatal Stress and Fetal Sex. Am. J. Respir. Crit. Care. Med. 2017, 196, 1396–1403.
- 33.Perera, F.P.; Wang, S.; Rauh, V.; et al. Prenatal exposure to air pollution, maternal psychological distress, and child behavior. Pediatrics 2013, 132, e1284–e1294.
- 34.Vesterinen, H.M.; Morello-Frosch, R.; Sen, S.; et al. Cumulative effects of prenatal-exposure to exogenous chemicals and psychosocial stress on fetal growth: Systematic-review of the human and animal evidence. PLoS ONE 2017, 12, e0176331.
- 35.Lu, C.; Yang, W.; Wang, F.; et al. Effects of Intrauterine and post-natal exposure to air pollution on children’s pneumonia: key roles in different particulate matters exposure during critical time windows. J. Hazard. Mater. 2023, 457, 131837.
- 36.Lu, C.; Deng, W.; Qiao, Z.; et al. Childhood Helicobacter pylori infection: Impacts of environmental exposures and parental stress. J. Hazard. Mater. 2024, 478, 135584.
- 37.Lu, C.; Xiao, X.; Deng, W.; et al. Parental stress modifies effects of early life exposure to interior environmental factors and extraventricular air pollution on childhood otitis media. Build. Environ. 2025, 269, 112440.
- 38.Noble, K.G.; Houston, S.M.; Brito, N.H.; et al. Family income, parental education and brain structure in children and adolescents. Nat. Neurosci. 2015, 18, 773–778.
- 39.Gyamfi, P.; Brooks-Gunn, J.; Jackson, A.P. Associations between employment and financial and parental stress in low-income single black mothers. Women Health 2001, 32, 119–135.
- 40.Fujiwara, T.; Ito, J.; Kawachi, I. Income inequality, parental socioeconomic status, and birth outcomes in Japan. Am. J. Epidemiol. 2013, 177, 1042–1052.
- 41.Hakulinen, C.; Mok, P.L.; Horsdal, H.T.; et al. Parental income as a marker for socioeconomic position during childhood and later risk of developing a secondary care-diagnosed mental disorder examined across the full diagnostic spectrum: a national cohort study. BMC Med. 2020, 18, 323.
- 42.Chaudhuri, A.; Behan, P.O. Fatigue in neurological disorders. Lancet 2004, 363, 978–988.
- 43.Grossoehme, D.H.; Friebert, S.; Baker, J.N.; et al. Association of religious and spiritual factors with patient-reported outcomes of anxiety, depressive symptoms, fatigue, and pain interference among adolescents and young adults with cancer. JAMA Netw. Open 2020, 3, e206696.
- 44.Lock, A.M.; Bonetti, D.L.; Campbell, A.D. The psychological and physiological health effects of fatigue. Occup. Med. 2018, 68, 502–511.
- 45.Pawlikowska, T.; Chalder, T.; Hirsch, S.R.; et al. Population based study of fatigue and psychological distress. BMJ 1994, 308, 763–766.
- 46.Holroyd, K.A.; O’Donnell, F.J.; Stensland, M.; et al. Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: a randomized controlled trial. JAMA 2001, 285, 2208–2215.
- 47.McGeary, D.D.; Resick, P.A.; Penzien, D.B.; et al. Cognitive behavioral therapy for veterans with comorbid posttraumatic headache and posttraumatic stress disorder symptoms: a randomized clinical trial. JAMA Neurol. 2022, 79, 746–757.
- 48.Schramm, S.H.; Moebus, S.; Lehmann, N.; et al. The association between stress and headache: A longitudinal population-based study. Cephalalgia 2015, 35, 853–863.
- 49.Sic, A.; Bogicevic, M.; Brezic, N.; et al. Chronic stress and headaches: the role of the HPA axis and autonomic nervous system. Biomedicines 2025, 13, 463.
- 50.Espay, A.J.; Aybek, S.; Carson, A.; et al. Current concepts in diagnosis and treatment of functional neurological disorders. JAMA Neurol. 2018, 75, 1132–1141.
- 51.Möhrenschlager, M.; Schäfer, T.; Huss-Marp, J.; et al. The course of eczema in children aged 5–7 years and its relation to atopy: differences between boys and girls. Br. J. Dermatol. 2006, 154, 505–513.
- 52.Ek, W.E.; Karlsson, T.; Hernándes, C.A.; et al. Breast-feeding and risk of asthma, hay fever, and eczema. J. Allergy Clin. Immunol. 2018, 141, 1157–1159.
- 53.Calov, M.; Alinaghi, F.; Hamann, C.R.; et al. The association between season of birth and atopic dermatitis in the northern hemisphere: a systematic review and meta-analysis. J. Allergy Clin. Immunol. Pract. 2020, 8, 674–680.
- 54.Lee, Y.L.; Li, C.W.; Sung, F.C.; et al. Environmental factors, parental atopy and atopic eczema in primary-school children: a cross-sectional study in Taiwan. Br. J. Dermatol. 2007, 157, 1217–1224.
- 55.Nafstad, P.; Magnus, P.; Gaarder, P.I.; et al. Exposure to pets and atopy-related diseases in the first 4 years of life. Allergy 2001, 56, 307–312.
- 56.Acabchuk, R.L.; Kamath, J.; Salamone, J.D.; et al. Stress and chronic illness: The inflammatory pathway. Soc. Sci. Med. 2017, 185, 166–170.
- 57.Bockelbrink, A.; Heinrich, J.; Schäfer, I.; et al. Atopic eczema in children: another harmful sequel of divorce. Allergy 2006, 61, 1397–1402.
- 58.Calam, R.; Gregg, L.; Simpson, A.; et al. Behavior problems antecede the development of wheeze in childhood: a birth cohort study. Am. J. Respir. Crit. Care. Med. 2005, 171, 323–327.
- 59.Sandberg, S.; Paton, J.Y.; Ahola, S.; et al. The role of acute and chronic stress in asthma attacks in children. Lancet 2000, 356, 982–987.
- 60.Wen, H.J.; Wang, Y.J.; Lin, Y.C.; et al. Prediction of atopic dermatitis in 2-yr-old children by cord blood IgE, genetic polymorphisms in cytokine genes, and maternal mentality during pregnancy. Pediatr. Allergy Immunol. 2011, 22, 695–703.
- 61.Sausenthaler, S.; Rzehak, P.; Chen, C.M.; et al. Stress-related maternal factors during pregnancy in relation to childhood eczema: results from the LISA Study. J. Investig. Allergol. Clin. Immunol. 2009, 19, 481–487.
- 62.Stefanovic, N.; Irvine, A.D.; Flohr, C. The Role of the Environment and Exposome in Atopic Dermatitis. Curr. Treat. Options Allergy 2021, 8, 222–241.
- 63.El-Heis, S.; Crozier, S.R.; Healy, E.; et al. Maternal stress and psychological distress preconception: association with offspring atopic eczema at age 12 months. Clin. Exp. Allergy 2017, 47, 760–769.
- 64.Wang, I.J.; Wen, H.J.; Chiang, T.L.; et al. Maternal employment and atopic dermatitis in children: a prospective cohort study. Br. J. Dermatol. 2013, 168, 794–801.
- 65.Garcia-Marcos, L.; Robertson, C.F.; Ross Anderson, H.; et al. Does migration affect asthma, rhinoconjunctivitis and eczema prevalence? Global findings from the international study of asthma and allergies in childhood. Int. J. Epidemiol. 2014, 43, 1846–1854.
- 66.Chang, H.Y.; Suh, D.I.; Yang, S.I.; et al. Prenatal maternal distress affects atopic dermatitis in offspring mediated by oxidative stress. J. Allergy Clin. Immunol. 2016, 138, 468–475.
- 67.Ai, Y.; Huang, J.; Zhu, T.T. Early exposure to maternal stress and risk for atopic dermatitis in children: a systematic review and meta-analysis. Clin. Transl. Allergy 2024, 14, e12346.
- 68.Chan, C.W.; Law, B.M.; Liu, Y.H.; et al. The association between maternal stress and childhood eczema: a systematic review. Int. J. Environ. Res. Public Health 2018, 15, 395.
- 69.Ramirez, F.D; Chen, S.; Langan, S.M.; et al. Assessment of Sleep Disturbances and Exhaustion in Mothers of Children With Atopic Dermatitis. JAMA Dermatol. 2019, 155, 556.
- 70.Kuo, H.C.; Chang, L.S.; Tsai, Z.Y.; et al. Allergic diseases do not impair the cognitive development of children but do damage the mental health of their caregivers. Sci. Rep. 2020, 10, 13854.
- 71.Bornehag, C.G.; Sundell, J.; Hägerhed-Engman, L.; et al. Association between ventilation rates in 390 Swedish homes and allergic symptoms in children. Indoor Air 2005, 15, 275–280.
- 72.Herbarth, O; Fritz, G.J.; Rehwagen, M.; et al. Association between indoor renovation activities and eczema in early childhood. Int. J. Hyg. Environ. Health 2006, 209, 241–247.
- 73.Lee, J.H.; Suh, J.; Kim, E.H.; et al. Surveillance of home environment in children with atopic dermatitis: a questionnaire survey. Asia Pac. Allergy 2012, 2, 59–66.
- 74.Lee, J.Y.; Seo, J.H.; Kwon, J.W.; et al. Exposure to gene-environment interactions before 1 year of age may favor the development of atopic dermatitis. Int. Arch. Allergy Immunol. 2012, 157, 363–371.
- 75.Carson, C.G.; Rasmussen, M.A.; Thyssen, J.P.; et al. Clinical presentation of atopic dermatitis by filaggrin gene mutation status during the first 7 years of life in a prospective cohort study. PLoS ONE 2012, 7, e48678.
- 76.Kim, E.H.; Kim, S.; Lee, J.H.; et al. Indoor air pollution aggravates symptoms of atopic dermatitis in children. PLoS ONE 2015, 10, e0119501.
- 77.Neuman, Å.; Hohmann, C.; Orsini, N.; et al. Maternal smoking in pregnancy and asthma in preschool children: a pooled analysis of eight birth cohorts. Am. J. Respir. Crit. Care Med. 2012, 186, 1037–1043.
- 78.Lee, J.H.; Son, S.W.; Cho, S.H. A Comprehensive Review of the Treatment of Atopic Eczema. Allergy Asthma Immunol. Res. 2016, 8, 181-190.
- 79.Ständer, S. Atopic Dermatitis. N. Engl. J. Med. 2021, 384, 1136–1143.
- 80.Egawa, M.; Kohno, Y.; Kumano, Y. Oxidative effects of cigarette smoke on the human skin. Int. J. Cosmet. Sci. 1999, 21, 83–98.
- 81.Krämer, U.; Lemmen, C.H.; Behrendt, H.; et al. The effect of environmental tobacco smoke on eczema and allergic sensitization in children. Br. J. Dermatol. 2004, 150, 111–118.
- 82.Wickman, M.; Melén, E.; Berglind, N.; et al. Strategies for preventing wheezing and asthma in small children. Allergy 2003, 58, 742–747.
- 83.Leung, D.Y.; Guttman-Yassky, E. Deciphering the complexities of atopic dermatitis: shifting paradigms in treatment approaches. J. Allergy Clin. Immunol. 2014, 134, 769–779.
- 84.Kim, J.; Kim, E.H.; Oh, I.; et al. Symptoms of atopic dermatitis are influenced by outdoor air pollution. J. Allergy Clin. Immunol. 2013, 132, 495–498.
- 85.Guo, Q.; Liang, F.; Tian, L.; et al. Ambient air pollution and the hospital outpatient visits for eczema and dermatitis in Beijing: a time-stratified case-crossover analysis. Environ. Sci. Process Impacts 2019, 21, 163–173.
- 86.Gref, A.; Merid, S.K.; Gruzieva, O.; et al. Genome-Wide Interaction Analysis of Air Pollution Exposure and Childhood Asthma with Functional Follow-up. Am. J. Respir. Crit. Care Med. 2017, 195, 1373–1383.
- 87.Ushio, H.; Nohara, K.; Fujimaki, H. Effect of environmental pollutants on the production of pro-inflammatory cytokines by normal human dermal keratinocytes. Toxicol. Lett. 1999, 105, 17–24.
- 88.Huss-Marp, J.; Eberlein-König, B.; Breuer, K.; et al. Influence of short-term exposure to airborne Der p 1 and volatile organic compounds on skin barrier function and dermal blood flow in patients with atopic eczema and healthy individuals. Clin. Exp. Allergy 2006, 36, 338–345.
- 89.Kim, B.E.; Leung, D.Y.M. Significance of Skin Barrier Dysfunction in Atopic Dermatitis. Allergy Asthma Immunol. Res. 2018, 10, 207–215.
- 90.Deng, S.; Huang, D.; Wang, W.; et al. Associations of gestational and the first year of life exposure to ambient air pollution with childhood eczema in Hubei, China. Environ. Sci. Pollut. Res. Int. 2019, 26, 23842–23849.
- 91.Boguniewicz, M.; Leung, D.Y. Recent insights into atopic dermatitis and implications for management of infectious complications. J. Allergy Clin. Immunol. 2010, 125, 4–13.
- 92.Joshi, P.A.; Smith, J.; Vale, S.; et al. The Australasian Society of Clinical Immunology and Allergy infant feeding for allergy prevention guidelines. Med. J. Aust. 2019, 210, 89–93.
- 93.Thomsen, S.F. Atopic dermatitis: natural history, diagnosis, and treatment. ISRN Allergy 2014, 2014, 354250.
- 94.Maintz, L.; Novak, N. Getting more and more complex: the pathophysiology of atopic eczema. Eur. J. Dermatol. 2007, 17, 267–283.
- 95.Lu, C.; Jiang, Y.; Deng, W.; et al. Early-life nutritional additives, household environment, and air pollution in relation to childhood food allergies: A multi-city mother–child study in China. Environ. Int. 2025, 203, 109774.

This work is licensed under a Creative Commons Attribution 4.0 International License.