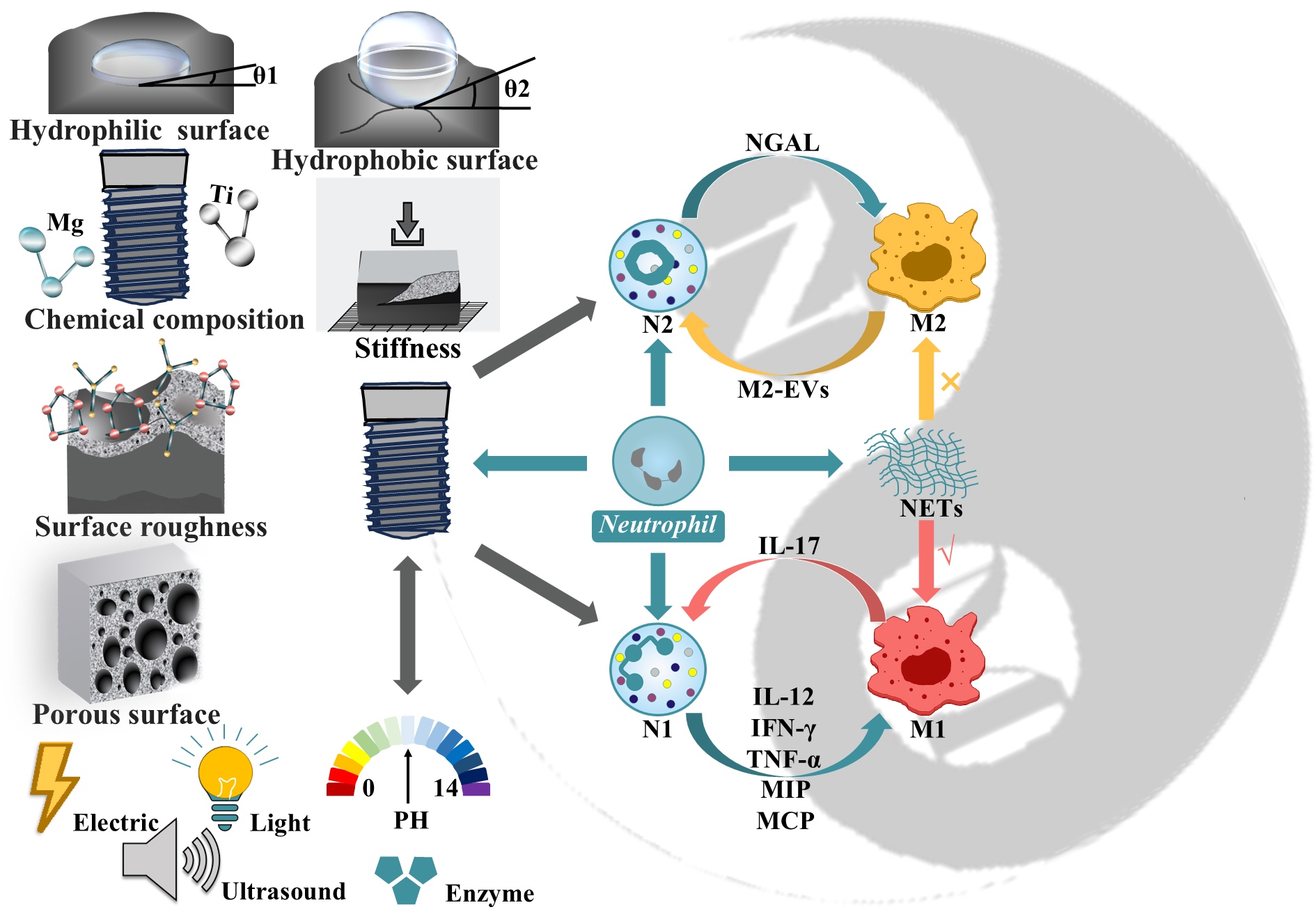
Neutrophils are the most abundant leukocytes and primary immune defenders in humans. Emerging evidence pinpoints that neutrophils possess a functional spectrum, mirroring macrophage polarization, spanning pro-inflammatory (N1) to anti-inflammatory/reparative (N2) phenotypes, contributing pivotally to host defense and immune modulation. In this Perspective, we first summarize the classification criteria, defining markers, and functional relevance of neutrophil polarization, highlighting their dynamic crosstalk with macrophages in shaping local immune microenvironments. Merging latest advances in immunology and biomaterials science, we move on to discuss how neutrophil-directed immunomodulation is informing the design of bioadaptive dental implants that feature tailored surface properties (chemistry, topography, wettability, etc.) to spatiotemporally steer neutrophil responses, aiming at alleviating foreign body reaction, controlling inflammation, and expediting osseointegration. The ultimate goal here is to provide guidance for designing bioadaptive implants with active immunoregulation targeting neutrophil–material interplays for tackling compromised osseointegration in dental implantation.
- Open Access
- Perspective
Neutrophil Polarization and Immune Regulation: Toward Immune-Bioadaptive Dental Implants
Author Information
Received: 09 Nov 2025 | Revised: 24 Nov 2025 | Accepted: 02 Dec 2025 | Published: 08 Dec 2025
Abstract
Graphical Abstract
References
- 1.
Jia, Z.; Xu, X.; Zhu, D.; et al. Design, printing, and engineering of regenerative biomaterials for personalized bone healthcare. Prog. Mater. Sci. 2023, 134, 101072.
- 2.
Hotchkiss, K.M.; Reddy, G.B.; Hyzy, S.L.; et al. Titanium surface characteristics, including topography and wettability, alter macrophage activation. Acta. Biomater. 2016, 31, 425–434.
- 3.
Xu, X.; Jia, Z.; Zheng, Y.; et al. Bioadaptability of biomaterials: aiming at precision medicine. Matter 2021, 4, 2648–2650.
- 4.
McWhorter, F.Y.; Wang, T.; Nguyen, P.; et al. Modulation of macrophage phenotype by cell shape. Proc. Natl. Acad. Sci. USA 2013, 110, 17253–17258.
- 5.
Guo, X.; Li, J.; Wu, Y.; et al. Recent advancements in hydrogels as novel tissue engineering scaffolds for dental pulp regeneration. Int. J. Biol. Macromol. 2024, 264, 130708.
- 6.
Sorsa, T.; Tjäderhane, L.; Konttinen, Y.T.; et al. Matrix metalloproteinases: contribution to pathogenesis, diagnosis and treatment of periodontal inflammation. Ann. Med. 2006, 38, 306–321.
- 7.
Chen, B.; Wang, W.; Hu, M.; et al. “Photo-thermo-electric” dental implant for anti-Infection and enhanced osteoimmunomodulation. ACS Nano 2024, 18, 24968–24983.
- 8.
Soehnlein, O.; Lindbom, L. Phagocyte partnership during the onset and resolution of inflammation. Nat. Rev. Immunol. 2010, 10, 427–439.
- 9.
Rosales, C. Neutrophil: A cell with many roles in inflammation or several cell types? Front. Physiol. 2018, 9, 113.
- 10.
Nathan, C. Neutrophils and immunity: challenges and opportunities. Nat. Rev. Immunol. 2006, 6, 173–182.
- 11.
Deniset, J.F.; Kubes, P. Neutrophil heterogeneity: bona fide subsets or polarization states? J. Leukoc. Biol. 2018, 103, 829–838.
- 12.
Fridlender, Z.G.; Sun, J.; Kim, S.; et al. Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer Cell 2009, 16, 183–194.
- 13.
Fine, N.; Hassanpour, S.; Borenstein, A.; et al. Distinct oral neutrophil subsets define health and periodontal disease states. J. Dent. Res. 2016, 95, 931–938.
- 14.
Xie, X.; Shi, Q.; Wu, P.; et al. Single-cell transcriptome profiling reveals neutrophil heterogeneity in homeostasis and infection. Nat. Immunol. 2020, 21, 1119–1133.
- 15.
Sansores-Espana, L.D.; Melgar-Rodriguez, S.; Vernal, R.; et al. Neutrophil N1 and N2 subsets and their possible association with periodontitis: a scoping review. Int. J. Mol. Sci. 2022, 23, 12068.
- 16.
Ma, Y.; Yabluchanskiy, A.; Iyer, R.P.; et al. Temporal neutrophil polarization following myocardial infarction. Cardiovasc. Res. 2016, 110, 51–61.
- 17.
Silvestre-Roig, C.; Hidalgo, A.; Soehnlein, O. Neutrophil heterogeneity: implications for homeostasis and pathogenesis. Blood 2016, 127, 2173–2181.
- 18.
Ohms, M.; Moller, S.; Laskay, T. An attempt to polarize human neutrophils toward N1 and N2 phenotypes in vitro. Front. Immunol. 2020, 11, 532.
- 19.
Mihaila, A.C.; Ciortan, L.; Macarie, R.D.; et al. Transcriptional profiling and functional analysis of N1/N2 neutrophils reveal an immunomodulatory effect of S100A9-blockade on the pro-inflammatory N1 subpopulation. Front. Immunol. 2021, 12, 708770.
- 20.
Ge, M.; Zhu, W.; Mei, J.; et al. Piezoelectric-enhanced nanocatalysts trigger neutrophil N1 polarization against bacterial biofilm by disrupting redox homeostasis. Adv. Mater. 2025, 37, e2409633.
- 21.
Neely, C.J.; Kartchner, L.B.; Mendoza, A.E.; et al. Flagellin treatment prevents increased susceptibility to systemic bacterial infection after injury by inhibiting anti-inflammatory IL-10+ IL-12-neutrophil polarization. PLoS ONE 2014, 9, e85623.
- 22.
Mizuno, R.; Kawada, K.; Itatani, Y.; et al. The role of tumor-associated neutrophils in colorectal cancer. Int. J. Mol. Sci. 2019, 20, 529.
- 23.
Cuartero, M.I.; Ballesteros, I.; Moraga, A.; et al. N2 neutrophils, novel players in brain inflammation after stroke: modulation by the PPARgamma agonist rosiglitazone. Stroke 2013, 44, 3498–3508.
- 24.
Yang, J.; Xie, Y.; Xia, Z.; et al. HucMSC-Exo induced N2 polarization of neutrophils: implications for angiogenesis and tissue restoration in wound healing. Int. J. Nanomed. 2024, 19, 3555–3575.
- 25.
Huang, S.; Xie, Y.; Zhan, Z.; et al. Geranyl hydroquinone alleviates rheumatoid arthritis-associated pain by suppressing neutrophil accumulation, N1 polarization and ROS production in mice. Redox Biol. 2025, 82, 103603.
- 26.
Jiang, Q.; Zhao, Y.; Shui, Y.; et al. Interactions between neutrophils and periodontal pathogens in late-onset periodontitis. Front. Cell. Infect. Microbiol. 2021, 11, 627328.
- 27.
Chaney, S.; Vergara, R.; Qiryaqoz, Z.; et al. The involvement of neutrophils in the pathophysiology and treatment of osteoarthritis. Biomedicines 2022, 10, 1604.
- 28.
Liu, L.; Wen, Y.; Chen, L.; et al. Xenogenous implanted dental follicle stem cells promote periodontal regeneration through inducing the N2 phenotype of neutrophils. Stem Cell Res. Ther. 2024, 15, 270.
- 29.
Antuamwine, B.B.; Bosnjakovic, R.; Hofmann-Vega, F.; et al. N1 versus N2 and PMN-MDSC: a critical appraisal of current concepts on tumor-associated neutrophils and new directions for human oncology. Immunol. Rev. 2023, 314, 250–279.
- 30.
He, Y.; Qu, Y.; Jin, S.; et al. ALDH3A1 upregulation inhibits neutrophils N2 polarization and halts oral cancer growth. Oral Dis. 2024, 30, 4231–4242.
- 31.
He, W.; Yan, L.; Hu, D.; et al. Neutrophil heterogeneity and plasticity: unveiling the multifaceted roles in health and disease. MedComm 2025, 6, e70063.
- 32.
Cai, B.; Lin, D.; Li, Y.; et al. N2-polarized neutrophils guide bone mesenchymal stem cell recruitment and initiate bone regeneration: a missing piece of the bone regeneration puzzle. Adv. Sci. 2021, 8, e2100584.
- 33.
Lehnfeld, J.; Dukashin, Y.; Mark, J.; et al. Saliva and serum protein adsorption on chemically modified silica surfaces. J. Dent. Res. 2021, 100, 1047–1054.
- 34.
Aseri, A.A. Exploring the role of artificial intelligence in dental implantology: a scholarly review. J. Pharm. Bioallied Sci. 2025, 17, S102–S104.
- 35.
Zhang, Q.; Luo, X.; Liu, K.; et al. Injectable cationic dynamic hydrogel with supramolecular drug loading reprograms neutrophil fate to alleviate diabetic periodontitis. Mater. Today Bio 2025, 35, 102557.
- 36.
Yao, Y.; Yin, Y.; Shuai, F.; et al. M2 macrophage-derived extracellular vesicles reprogram immature neutrophils into Anxa1hi neutrophils to enhance inflamed bone regeneration. Adv. Sci. 2025, 12, e2416159.
- 37.
Horckmans, M.; Ring, L.; Duchene, J.; et al. Neutrophils orchestrate post-myocardial infarction healing by polarizing macrophages towards a reparative phenotype. Eur. Heart J. 2017, 38, 187–197.
- 38.
Huţanu, A.; Iancu, M.; Bălaşa, R; et al. Predicting functional outcome of ischemic stroke patients in Romania based on plasma CRP, sTNFR-1, D-Dimers, NGAL and NSE measured using a biochip array. Acta Pharmacol. Sin. 2018, 39, 1228–1236.
- 39.
Wang, W.; Zheng, C.; Yang, J.; et al. Intersection between macrophages and periodontal pathogens in periodontitis. J. Leukoc. Biol. 2021, 110, 577–583.
- 40.
Kourtzelis, I.; Hajishengallis, G.; Chavakis, T. Phagocytosis of apoptotic cells in resolution of inflammation. Front. Immunol. 2020, 11, 553.
- 41.
Yona, S.; Kim, K.W.; Wolf, Y.; et al. Fate mapping reveals origins and dynamics of monocytes and tissue macrophages under homeostasis. Immunity 2013, 38, 79–91.
- 42.
Biswas, S.K.; Mantovani, A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat. Immunol. 2010, 11, 889–896.
- 43.
Mesa-Restrepo, A.; Byers, E.; Brown, J.L.; et al. Osteointegration of Ti bone implants: a study on how surface parameters control the foreign body response. ACS Biomater. Sci. Eng. 2024, 10, 4662–4681.
- 44.
Sousa, A.B.; Barbosa, J.N. The role of neutrophils in biomaterial-based tissue repair-shifting paradigms. J. Funct. Biomater. 2023, 14, 327.
- 45.
Wang, J. Neutrophils in tissue injury and repair. Cell Tissue Res. 2018, 371, 531–539.
- 46.
Wei, X.; Lei, L.; Luo, L.; et al. Advances in osteoimmunomodulation of biomaterials after intrabone implantation: focus on surface hydrophilicity. J. Mater. Chem. B. 2024, 12, 11089–11104.
- 47.
Pierschbacher, M.D.; Ruoslahti, E. Cell attachment activity of fibronectin can be duplicated by small synthetic fragments of the molecule. Nature 1984, 309, 30–33.
- 48.
Cheresh, D.A.; Spiro, R.C. Biosynthetic and functional properties of an Arg-Gly-Asp-directed receptor involved in human melanoma cell attachment to vitronectin, fibrinogen, and von Willebrand factor. J. Biol. Chem. 1987, 262, 17703–17711.
- 49.
Moursi, A.M.; Damsky, C.H.; Lull, J.; et al. Fibronectin regulates calvarial osteoblast differentiation. J. Cell. Sci. 1996, 109, 1369–1380.
- 50.
Wilson, C.J.; Clegg, R.E.; Leavesley, D.I.; et al. Mediation of biomaterial-cell interactions by adsorbed proteins: a review. Tissue Eng. 2005, 11, 1–18.
- 51.
Nygren, H.; Tengvall, P.; Lundstrom, I. The initial reactions of TiO2 with blood. J. Biomed. Mater. Res. 1997, 34, 487–492.
- 52.
Swanson, K.V.; Deng, M.; Ting, J.P. The NLRP3 inflammasome: Molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 2019, 19, 477–489.
- 53.
Abaricia, J.O.; Shah, A.H.; Musselman, R.M.; et al. Hydrophilic titanium surfaces reduce neutrophil inflammatory response and NETosis. Biomater. Sci. 2020, 8, 2289–2299.
- 54.
Schlaepfer, D.D.; Hanks, S.K.; Hunter, T.; et al. Integrin-mediated signal transduction linked to Ras pathway by GRB2 binding to focal adhesion kinase. Nature 1994, 372, 786–791.
- 55.
Jiang, T.; Tang, X.Y.; Mao, Y.; et al. Matrix mechanics regulate the polarization state of bone marrow-derived neutrophils through the JAK1/STAT3 signaling pathway. Acta. Biomater. 2023, 168, 159–173.
- 56.
Rupp, F.; Liang, L.; Geis-Gerstorfer, J.; et al. Surface characteristics of dental implants: A review. Dent. Mater. 2018, 34, 40–57.
- 57.
Xiu, P.; Jia, Z.; Lv, J.; et al. Tailored surface treatment of 3D printed porous Ti6Al4V by microarc oxidation for enhanced osseointegration via optimized bone in-growth patterns and interlocked bone/implant interface. ACS Appl. Mater. Interfaces 2016, 8, 17964–17975.
- 58.
Dotta, T.C.; D’Ercole, S.; Iezzi, G.; et al. The interaction between oral bacteria and 3D titanium porous surfaces produced by selective laser melting-a narrative review. Biomimetics 2024, 9, 461.
- 59.
Jia, Z.; Xiu, P.; Li, M.; et al. Bioinspired anchoring AgNPs onto micro-nanoporous TiO2 orthopedic coatings: trap-killing of bacteria, surface-regulated osteoblast functions and host responses. Biomaterials 2016, 75, 203–222.
- 60.
Duan, Y.; An, W.; Wu, H.; et al. Salvianolic acid C attenuates LPS-induced inflammation and apoptosis in human periodontal ligament stem cells via Toll-like receptors 4 (TLR4)/nuclear factor kappa B (NF-kappaB) pathway. Med. Sci. Monit. 2019, 25, 9499–9508.
- 61.
Sun, J.Y.; Li, D.L.; Dong, Y.; et al. Baicalin inhibits toll-like receptor 2/4 expression and downstream signaling in rat experimental periodontitis. Int. Immunopharmacol. 2016, 36, 86–93.
- 62.
Hallab, N.J.; Mikecz, K.; Vermes, C.; et al. Differential lymphocyte reactivity to serum-derived metal-protein complexes produced from cobalt-based and titanium-based implant alloy degradation. J. Biomed. Mater. Res. 2001, 56, 427–436.
- 63.
Yue, J.; Jin, S.; Li, Y.; et al. Magnesium inhibits the calcification of the extracellular matrix in tendon-derived stem cells via the ATP-P2R and mitochondrial pathways. Biochem. Biophys. Res. Commun. 2016, 478, 314–322.
- 64.
Huang, C.; Sanaei, F.; Verdurmen, W.P.R.; et al. The application of organs-on-a-chip in dental, oral, and craniofacial research. J. Dent. Res. 2023, 102, 364–375.
- 65.
Ingber, D.E. Human organs-on-chips for disease modelling, drug development and personalized medicine. Nat. Rev. Genet. 2022, 23, 467–491.
- 66.
Delhalle, S.; Bode, S.F.N.; Balling, R.; et al. A roadmap towards personalized immunology. NPJ Syst. Biol. Appl. 2018, 4, 9.
- 67.
Koelzer, V.H.; Sirinukunwattana, K.; Rittscher, J.; et al. Precision immunoprofiling by image analysis and artificial intelligence. Virchows Arch. 2019, 474, 511–522.
- 68.
Vasudevan, K.T.D.; Hebbar, S.R.; Selvam, P.K.; et al. Multi-omics and AI-driven immune subtyping to optimize neoantigen-based vaccines for colorectal cancer. Sci. Rep. 2025, 15, 19333.

This work is licensed under a Creative Commons Attribution 4.0 International License.