- Multidisciplinary evidence linking environmental degradation and human health
- Amplified vector-borne diseases, foodinsecurity, and heat-related morbidity
- Community-levelengagement, real-time data, and AI-enabled decision support can enhance climate preparedness and health system responsiveness.
- Open Access
- Review
Climate Change, Environmental Degradation, and Human Health: A Converging Crisis
- Ajith Kumar S. Nair 1, *,
- Yau Adamu 2,
- Hugh Montgomery 3, 4,
- Gurleen Kaur 5,
- Manmeet Singh 6,
- Naveen Sudharsan 7,
- Yun Hang 8
Author Information
Received: 04 Nov 2025 | Revised: 22 Nov 2025 | Accepted: 17 Dec 2025 | Published: 05 Jan 2026
Highlights
Abstract
Graphical Abstract
References
- 1.
World Health Organization. Climate Change and Health; WHO: Geneva, Switzerland, 2018.
- 2.
Intergovernmental Panel on Climate Change (IPCC). Climate Change 2023: Synthesis Report. Contribution of Working Groups I, II, and III to the Sixth Assessment Report of the IPCC ; Core Writing Team, Lee, H., Romero, J., Eds.; IPCC: Geneva, Switzerland, 2023.
- 3.
Myers, S.S.; Gaffikin, L.; Golden, C.D.; et al. Human health impacts of ecosystem alteration. Proc. Natl. Acad. Sci. USA 2013, 110, 18753–18760. https://doi.org/10.1073/pnas.121865611
- 4.
Whitmee, S.; Haines, A.; Beyrer, C.; et al. Safeguarding human health in the Anthropocene epoch: Report of the Rockefeller Foundation–Lancet Commission on planetary health. Lancet 2015, 386, 1973–2028. https://doi.org/10.1016/S0140-6736(15)60901-1
- 5.
Romanello, M.; Di Napoli, C.; Green, C.; et al. The 2023 report of the Lancet Countdown on health and climate change: Protecting health in a warming world. Lancet 2023, 402, 2346–2404. https://doi.org/10.1016/S0140-6736(23)01859-7
- 6.
United Nations Environment Programme (UNEP). Making Peace With Nature: A Scientific Blueprint to Tackle the Climate, Biodiversity and Pollution Emergencies; UNEP: Nairobi, Kenya, 2021.
- 7.
Montgomery, H. Final call Climate change and us. J. R. Coll. Physicians Edinb. 2024, 54, 101–104. https://doi.org/10.1177/14782715241239085
- 8.
Le Qur, C.; Jackson, R.B.; Jones, M.W.; et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat. Clim. Change 2020, 10, 647–653. https://doi.org/10.1038/s41558-020-0797-x
- 9.
Forster, P.M.; Forster, H.I.; Evans, M.J.; et al. Current and future global climate impacts resulting from COVID-19. Nat. Clim. Change 2020, 10, 913–919. https://doi.org/10.1038/s41558-020-0883-0
- 10.
Mazdiyasni, O.; AghaKouchak, A.; Davis S.J.; et al. Increasing probability of mortality during Indian heat waves Sci. Adv. 2017, 3, e1700066. https://doi.org/10.1126/sciadv.1700066
- 11.
Sarath Chandran, M.A.; Subba Rao, A.V.M.; Sandeep, V.M.; et al. Indian summer heat wave of 2015: A biometeorological analysis using half hourly automatic weather station data with special reference to Andhra Pradesh. Int. J. Biometeorol. 2017, 61, 1063–1072. https://doi.org/10.1007/s00484-016-1286-9
- 12.
Mourougan, M.; Tiwari, A.; Limaye, V.; et al. Heat stress in India: A review. Prev. Med. Res. Rev. 2024, 1, 140–147. https://doi.org/10.4103/PMRR.PMRR_100_23
- 13.
Ghatak, D.; Zaitchik, B.; Hain, C.; et al. The role of local heating in the 2015 Indian heat wave. Sci. Rep. 2017, 7, 7707. https://doi.org/10.1038/s41598-017-07956-5
- 14.
Neethu, C; Ramesh, K.V. Projected changes in heat wave characteristics over India. Clim. Change 2023, 176, 144. https://doi.org/10.1007/s10584-023-03618-w
- 15.
Satyanarayana, G.C.; Velivelli, S.; Rao, K.K.; et al. Increasing heat wave frequencies over India during post-El Niño spring and ˜early summer seasons. Glob. Planet. Change 2024, 241, 104561. https://doi.org/10.1016/j.gloplacha.2024.104561
- 16.
Ratnam, J.V.; Behera, S.K.; Ratna, S.B.; et al. Anatomy of Indian heat waves. Sci. Rep. 2016, 6, 24395. https://doi.org/10.1038/srep24395
- 17.
Rohini, P.; Rajeevan, M.; Srivastava, A.K.; et al. Variability & trends of India heat waves. Sci. Rep. 2016, 6, 26153. https://doi.org/10.1038/srep26153
- 18.
India Meteorological Department (IMD). Heat Wave Watch Bulletin; India Meteorological Department: New Delhi, India, 2013.
- 19.
Dietz, L.R.; Chatterjee, S. Investigation of Precipitation Thresholds in the Indian Monsoon; Springer: Cham, Switzerland, 2015; pp. 239– 246.
- 20.
Zhu, K.; Yang, Y.; Xue, M.; et al. Neighborhood precipitation verification. Adv. Atmos. Sci. 2015, 32, 1449–1459. https://doi.org/10.1007/s00376-015-5023-9
- 21.
Perkins, S.E.; Alexander, L.V. Measurement of heat waves. J. Climate 2013, 26, 4500–4517. https://doi.org/10.1175/JCLI-D-12-00383.1
- 22.
Loridan, T.; Coates, L.; Argeso, D.; et al. The excess heat factor for fatalities. Aust. J. Emerg. Manage. 2016, 31, 31–37.
- 23.
World Bank. Poverty & Vulnerability Indicators – India. World Bank: Washington, DC, USA, 2024.
- 24.
Sharma, A.; Dutta, P.; Shah, P.; et al. Extreme heat mortality Ahmedabad. Urban Clim. 2024, 54, 101832. https://doi.org/10.1016/j.uclim.2024.101832
- 25.
Vieira, R.F.C.; Muoz-Leal, S.; Faulkner, G.; et al. Global climate change impacts on vector ecology and vectorborne diseases. In Modernizing Global Health Security to Prevent, Detect, and Respond; McNabb, S.J.N.; Shaikh, A.T. and Haley, C.J., Eds.; Elsevier: Amsterdam, The Netherlands, 2024; pp. 155–173
- 26.
de Souza, W.M.; Weaver, S.C. Effects of climate change and human activities on vector-borne diseases. Nat. Rev. Microbiol. 2024, 22, 476–491. https://doi.org/10.1038/s41579-024-01026-0
- 27.
Siraj, A.S.; Santos-Vega, M.; Bouma, M.J.; et al. Altitudinal changes in malaria incidence in highlands of Ethiopia and Colombia. Science 2014, 343, 1154–1158. https://doi.org/10.1126/science.1244325
- 28.
Heidecke, J.; Wallin, J.; Fransson, P.; et al. Uncovering temperature sensitivity of West Nile virus transmission: Novel computational approaches to mosquito-pathogen trait responses. PLOS Comput. Biol. 2025, 21, e1012866. https://doi.org/10.1371/journal.pcbi.1012866
- 29.
Kaur, G.; Ghoshal, S.; Singh, M.; et al. EpiClim: Weekly DistrictWise all-India multi-epidemics Climate-Health Dataset for accelerated Geo Health research. arXiv 2025, arXiv:2501.18602v1
- 30.
Food and Agriculture Organization of the United Nations (FAO); International Fund for Agricultural Development (IFAD); United Nations Children’s Fund (UNICEF); World Food Programme (WFP); World Health Organization (WHO). The State of Food Security and Nutrition in the World 2024 – Financing to End Hunger, Food Insecurity and Malnutrition in All Its Forms; FAO: Rome, Italy, 2024.
- 31.
Health Effects Institute (HEI); Institute for Health Metrics and Evaluation (IHME). State of Global Air 2024: A Special Report on Global Exposure to Air Pollution and Associated Health Impacts ; HEI: Boston, MA, USA, 2024.
- 32.
Holloway, T.; Bratburd, J.R.; Fiore A.; et al. Satellite data to support air quality assessment and management J. Air Waste Manag. Assoc. 2025, 75, 429–463. https://doi.org/10.1080/10962247.2025.2484153
- 33.
Sorek-Hamer, M.; Just, A.C.; Kloog, I.; et al. Satellite remote sensing in epidemiological studies. Curr. Opin. Pediatr. 2016, 28, 228–234. https://doi.org/10.1097/MOP.0000000000000326
- 34.
Lee, H.J. Advancing exposure assessment of PM2.5 using satellite remote sensing: A review. Asian J. Atmos. Environ. 2020, 14, 319–334. https://doi.org/10.5572/ajae.2020.14.4.319
- 35.
Stratoulias, D.; Nuthammachot, N,; Dejchanchaiwong, R.; et al. Recent developments in satellite remote sensing for air pollution surveillance in support of sustainable development goals. Remote Sens. 2024, 16, 2932. https://doi.org/10.3390/rs16162932
- 36.
Holloway, T.; Bratburd, K.; Fiore, A.; et al. Observing the Diurnal Variations of Ozone-NOx-VOC Chemistry Using the First Geostationary Satellite. Geophys. Res. Lett. 2025, 52, e2025GL116394. https://doi.org/10.1029/2025GL116394
- 37.
Clark, L.P.; Zilber, D.; Schmitt, C.; et al. A review of geospatial exposure models and approaches for health data integration. J. Exposure Sci. Environ. Epidemiol. 2025, 35, 131–148. https://doi.org/10.1038/s41370-024-00712-8
- 38.
Shan, X.; Casey, J.A.; Shearston, J.A.; et al. Methods for quantifying source-specific air pollution exposure to serve epidemiology, risk assessment, and environmental justice. Geo Health 2024, 8, e2024GH001188. https://doi.org/10.1029/2024GH001188
- 39.
Romanello, M.; Walawender, M.; Hsu, S.-C.; et al. The 2024 report of the Lancet Countdown on health and climate change: facing recordbreaking threats from delayed action. Lancet 2024, 404, 1847–1896. https://doi.org/10.1016/S0140-6736(24)01822-1
- 40.
Cunsolo, A.; Ellis, N.R. Ecological grief as a mental health response to climate change–related loss. Nat. Clim. Change 2018, 8, 275–281. https://doi.org/10.1038/s41558-018-0092-2
- 41.
Berrang-Ford, L.; Sietsma, A.J.; Callaghan, M.W.; et al. Systematic mapping of global research on climate and health: A machine learning review. Lancet Planet. Health 2021, 5, e514–e525. https://doi.org/10.1016/S2542-5196(21)00179-0
- 42.
World Bank Group. Groundswell - Preparing for Internal Climate Migration, 2024 Update; World Bank: Washington, DC, USA, 2024.
- 43.
International Organization for Migration (IOM): World Migration Report 2024; International Organization for Migration (IOM): Geneva, Switzerland, 2024.
- 44.
Acheampong, E.; Opoku, A. Climate change and migration in SubSaharan Africa: Pathways and policy responses. J. Environ. Migr. Stud. 2023, 18, 145–162.
- 45.
Intergovernmental Panel on Climate Change (IPCC). Climate Change 2022: Impacts, Adaptation, and Vulnerability ; Working Group II Contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2022.
- 46.
Montgomery, H. Parliamentary Science Paper ; Parliamentary and Scientific Committee: London, UK, 2024.
- 47.
Sharma, A.K.; Baliyan, P.; Kumar, P.; et al. Air pollution and public health in Delhi. Rev. Environ. Health 2018, 33, 77–86. https://doi.org/10.1515/reveh-2017-0032
- 48.
Xing, Y.-F.; Xu Y.-H.; Shi, M.-H.; et al. The impact of PM2.5 on the human respiratory system. J. Thorac. Dis. 2016, 8, E69–E74. https://doi.org/10.3978/j.issn.2072-1439.2016.01.19
- 49.
Kumar, S., Kumar, A.; Singh, M. Building climate-resilient health systems in India: A comprehensive health systems approach. Cureus 2024, 16, e68951. https://doi.org/10.7759/cureus.68951
- 50.
Salvi, S.; Kumar, G.A.; Dhaliwal, R.S.; et al. Burden of chronic respiratory diseases in India. Lancet Respir. Med. 2021, 9, 47–61.
- 51.
Dutta, A.; Jinsart, W. Air pollution in Delhi, India: It’s status and association with respiratory diseases. PLOS ONE 2022, 17, e0274444. https://doi.org/10.1371/journal.pone.0274444
- 52.
Singh, A.K.; Pathak, A.K.; Saubu, G. Premature mortality risk and associated economic loss assessment due to PM2.5 exposure in Delhi, India during 2015–2019. Air Qual. Atmos. Health 2024, 17, 1867–1883. https://doi.org/10.1007/s11869-024-01550-1
- 53.
Indian Council of Medical Research (ICMR). Climate and Health Database India: Technical Report ; ICMR: New Delhi, India, 2024.
- 54.
Delhi Pollution Control Committee (DPCC). Annual Air Quality Trends and Health Indicators; Delhi Report. DPCC: New Delhi, India, 2024.
- 55.
Tewari, P.; Ma, P.; Gan, G.; et al. Non-linear associations between meteorological factors, ambient air pollutants and major mosquitoborne diseases in Thailand. PLoS Negl. Trop. Dis. 2023, 17, e0011763. https://doi.org/10.1371/journal.pntd.0011763
- 56.
Air Quality Index (AQI). National Air Quality Bulletin. Ministry of Environment, Forest and Climate Change: New Delhi, India, 2025.
- 57.
Masih, I.; Maskey, S.; Muss, F.E.; et al. A review of droughts on the African continent: A geospatial and long-term perspective. Hydrol. Earth Syst. Sci., 2014, 18, 3635–3649. https://doi.org/10.5194/hess-18-3635-2014
- 58.
dos Santos, S.; Adams, E.A.; Neville, G.; et al. Urban growth & water access in Sub-Saharan Africa: Progress, challenges, and emerging research directions. Sci. Total Environ. 2017, 607–608, 497–508. https://doi.org/10.1016/j.scitotenv.2017.06.157
- 59.
Henderson, J.V.; Storeygard, A.; Deichmann, U. Has climate change driven urbanization in Africa? J. Dev. Econ. 2017, 124, 60–82. https://doi.org/10.1016/j.jdeveco.2016.09.001
- 60.
Dajuma, D.; Sylla, M.B.; Tall, M.; et al. Projected intensification and expansion of heat stress and related population exposure over Africa under future climates. Earths Futur. 2024, 12, e2024EF004646. https://doi.org/10.1029/2024EF004646
- 61.
Adeyeri, O.E.; Ajadi, S.A.; Ishola, K.A.; et al. The societal impact of heatwave intensification and heat stress on African urban populations. Soc. Imp. 2025, 6, 100148. https://doi.org/10.1016/j.socimp.2025.100148
- 62.
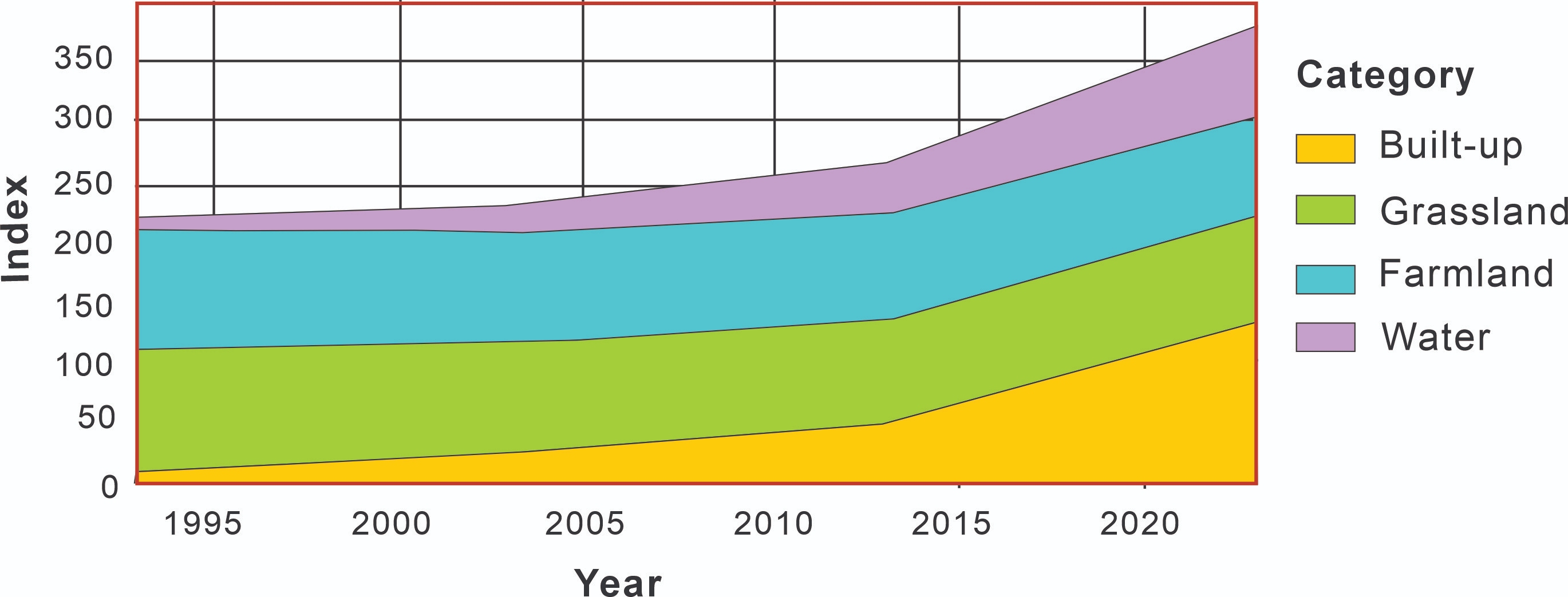
Yeboah, E.; Sarfo, I.; Zhu, Q.; et al. Traceability and projected patterns of Africa’s land use systems and climate vari-ability (1993–2053). Land Use Policy 2025, 157, 107680. https://doi.org/10.1016/j.landusepol.2025.107680
- 63.
Yahaya, I.; Xu, R.; Zhou, J.; et al. Projected patterns of land uses in Africa under a warming climate. Sci. Rep. 2024, 14, 12315. https://doi.org/10.1038/s41598-024-61035
- 64.
United Nations Children’s Fund (UNICEF). Children Displaced by Climate Impacts: WASH & Health Vulnerability Assessment ; UNICEF: New York, NY, USA, 2024.
- 65.
Africa CDC. Regional One Health Surveillance & Climate-sensitive Disease Systems; African Union/Africa CDC: Addis Ababa, Ethiopia, 2024.
- 66.
Network for Greening the Financial System. Climate Scenarios for Central Banks & Supervisors; NGFS: Paris, France, 2022.
- 67.
Steffen, W.; Richardson, K.; Rockstrm, J.; et al. Planetary boundaries: Guiding human development on a changing planet. Science 2015, 347, 1259855. https://doi.org/10.1126/science.1259855
- 68.
Burke, M.; Hsiang, S.M.; Miguel, E. Global non-linear effect of temperature on economic production. Nature 2015, 527, 235–239. https://doi.org/10.1038/nature15725
- 69.
Swiss Re Institute. The Economics of Climate Change: No Action Not an Option; Swiss Re Institute: Zurich, Switzerland, 2021.
- 70.
Kotz, M.; Levermann, A.; Wenz, L. The economic commitment of climate change. Nature 2024, 628, 551–557. https://doi.org/10.1038/s41586-024-07219-0
- 71.
Montgomery, H. Climate change impacts: Survival on, and of, intensive care. Crit. Care Rev. 2025, 29, 335. https://doi.org/10.1186/s13054-025-05565-7
- 72.
Piotrowski, M.; Nair, A.K.; Alpard, S.; et al. Application-based Digital Health Navigator ; SSRN: Rochester, NY, USA, 2025.
- 73.
Nair, A.S.; Suszanski, N.; Subramaniam, S.; et al. Leveraging Decision Intelligence and AI-driven Digital Health to Improve Patient Access and Reduce Readmissions in Oncology Care. 2025 (manuscript in preparation).
- 74.
Adamu, S.; Ibrahim, M.; Hassan, K.; et al. A One-Health early warning system for climate-driven harmful algal blooms. Sci Total Environ. 2025, 945, 173821. https://doi.org/10.1016/j.scitotenv.2025.173821
- 75.
Adamu, Y.; et al. ClimateDriven Harmful Algal Blooms: One Health System To Early Warning System (Draft 01) ; University of Texas Health Science Center: San Antonio, TX, USA, 2025.
- 76.
Townhill, B.L.; Tinker, J.; Jones, M.; et al. Harmful algal blooms and climate change: Exploring future distribution changes. ICES J. Mar. Sci. 2018, 75, 1882–1893. https://doi.org/10.1093/icesjms/fsy113
- 77.
Anderson, D.; Fensin, E.; Gobler, C.J.; et al. Marine harmful algal blooms in the United States: History, current status and future trends. Harmful Algae 2021, 102, 101975. https://doi.org/10.1016/j.hal.2021.101975
- 78.
Woods Hole Oceanographic Institution (WHOI). Harmful Algal Blooms & Climate Change: State of Knowledge ; WHOI Technical Report; Woods Hole Oceanographic Institution (WHOI): Woods Hole, MA, USA, 2024.
- 79.
Wang, Y.; Zhao, D.; Woolway, R.I.; et al. Global elevation of algal bloom frequency in large lakes over the past two decades. Nat. Sci. Rev. 2025, 12, nwaf011. https://doi.org/10.1093/nsr/nwaf011
- 80.
U.S. Army Corps of Engineers (USACE). ArcGIS HAB Explorer Data Summary; USACE Environmental Technical Report; U.S. Army Corps of Engineers (USACE): Washington, DC, USA, 2024.
- 81.
U.S. Environmental Protection Agency (EPA). HAB Monitoring and BloomWatch Public Reporting Framework ; EPA Public Health Report; U.S. Environmental Protection Agency (EPA): Washington, DC, USA, 2025.
- 82.
Rathore, A.; Singh, P.; Kumar, R. BloomSense: AI-driven early warning for HABs. J. Water Res. Technol. 2025, 41, 145–158.
- 83.
Limnotek/BloomOptix Inc. BloomOptix AI: AI-Assisted HAB Classification for Water Bodies ; Product Technical Whitepaper Limnotek/BloomOptix Inc.: Cleveland, OH, USA, 2025.
- 84.
HABTRAIL Consortium. HABTRAIL UAV–Microscopy Monitoring Platform for Freshwater HABs; Program Technical Overview; HABTRAIL Consortium: Lisbon, Portugal, 2025.
- 85.
Stolk, P.; Nyon, R. Integrated surveillance in One Health. EcoHealth 2017, 14, 523–531. https://doi.org/10.1007/s10393-017-1285-2
- 86.
Adenyi, T.; Musa, I.; Ojo, S. One Digital Health frameworks for integrated biosurveillance. Lancet Digital Health 2024, 6, e487–e499.
- 87.
Ho, C. Leveraging AI and big data for One Health surveillance. Comput. Health Sci. 2022, 8, 101–115.
- 88.
Benis, A.; Tamburis, O.; Chronaki, C.; et al. One digital health: A unified framework for health data integration. J. M. Internet Res. 2021, 23, e25715. https://doi.org/10.2196/22189
- 89.
Ahmed, S.; LePage, K.; Benc, R.; et al. Digital health platforms for participatory disease surveillance: Opportunities and challenges. Front. Public Health 2025, 13, 112345.
- 90.
Kim, J.; et al. IoT-enabled biosurveillance for zoonotic disease prevention. Int. J. Environ. Res. Public Health 2025, 22, 5678. https://doi.org/10.3390/ijerph22045678
- 91.
World Health Organization. Air Quality and Health; World Health Organization: Geneva, Switzerland, 2021. Available online: https://www.who.int/docs/default-source/documents/publications/air- quality-and-health.pdf (accessed on 2 January 2026).
- 92.
WMO & WHO. Climate & Health Data Must Be Integrated ; World Meteorological Organization (WMO) & World Health Organization (WHO): Geneva, Switzerland, 2024. Available online: https://wmo.int/media/news/climate-and-health-data-must-be- integrated (accessed on 2 January 2026).
- 93.
Bahrami, G.; Ghavidel, N.; Mahmoodi, Z.; et al. The health effects of climate change: Identifying strategies, policies, and knowledge gaps — An umbrella review. Int. J. Environ. Health Res. 2025, 1–18.
- 94.
World Health Organization. Health and Climate Change: A Briefing ; World Health Organization: Geneva, Switzerland, 2018.

This work is licensed under a Creative Commons Attribution 4.0 International License.