Erectile dysfunction (ED) is a prevalent male sexual dysfunction that can be categorized into organic and psychological forms. The organic type is further subdivided into neurogenic, vasogenic, drug-induced, and endocrine subtypes, among others. Risk factors for ED include smoking, obesity, diabetes, cardiovascular disease, and various psychological influences. Treatment strategies for managing the symptoms encompass lifestyle modifications, pharmacotherapy, physical therapy, stem cell therapy, and surgical interventions. Pharmacological options consist of phosphodiesterase inhibitors, testosterone, and α-adrenoceptor antagonists, while physical modalities include vacuum erection devices, prostaglandin E1 injection, and low-intensity extracorporeal shock wave therapy (LI-ESWT). Surgical procedures such as penile prosthesis implantation, are typically reserved for patients unsuited to non-surgical approaches or those experiencing adverse effects or unresponsiveness to medical therapy. This review elaborates on key aspects of ED, investigates diverse pathological mechanisms associated with the disorder, and outlines current treatment modalities.
- Open Access
- Review
Current Management of Erectile Dysfunction
- Siqi Wang 1,
- Haocheng Lin 2,3,
- Yan Zhang 1,4,5,6,7,*,
- Yahan Liu 1,*
Author Information
Received: 24 Sep 2024 | Revised: 12 Nov 2024 | Accepted: 13 Nov 2024 | Published: 08 Aug 2025
Abstract
Keywords
1.Introduction
Penile erection is a vital physiological process for sexual function. ED is characterized by the persistent and repeated inability to achieve or maintain an erection with sufficient rigidity and duration for satisfactory sexual intercourse [1], as defined by the International Consultation on Sexual Medicine (ICSM). The condition has a relatively high incidence rate and affects a diverse range of patients. However, despite the common prevalence of ED, our understanding of this condition remained had limited until the 1970s.
Historically, ED was primarily considered as a psychogenic disorder. Therefore, before the 1970s, the diagnostic evaluation of men with ED focused mainly on assessing their sexual psychology history and providing treatments that were primarily behavioral therapy. However, current evidence suggests that over 80% of ED cases have an organic etiology [2]. The World Health Organization emphasizes the importance of sexual health is in promoting the physical and emotional well-being of individuals, couples, families, and the social and economic development of communities and countries [3]. Regardless of its cause, ED can significantly impact mood, interpersonal relationships, and overall quality of life. This review aims to summarize the various etiologies of ED and the currently available treatments options.
2.Epidemiology
Previous literature has thoroughly demonstrated a positive correlation between the incidence rate of ED and age. A survey conducted in the United States revealed that 25.3% of individuals aged 45–54 and 33.9% of those aged 55–64 met the diagnostic criteria for ED, compared to 48.0% in the 65–74 age group and 52.2% in the 75 and older group [4]. Additionally, the Massachusetts Male Ageing Study (MMAS) is recognized as a seminal research effort that has produced noteworthy findings in this area. The MMAS, a community-based, random-sample prospective observational survey of men aged 40–70 years [5], identified an overall incidence rate of mild to moderate ED at 52%. Furthermore, the study emphasized the strong association of ED with age, emotional well-being, and health status. Research indicates that the ED prevalence is higher in the United States, East Asia, and Southeast Asian countries compared to Europe or South America. These regional disparities may be attributed to genetic and environmental factors. Furthermore, studies suggest that the global prevalence of ED could reach 322 million cases by 2025 [6]. However, there remains a scarcity of studies evaluating the worldwide prevalence of ED, potentially due to the underestimation resulting from societal taboos hindering individuals from seeking help.
With the increasing understanding of ED, awareness of its prevalence is also growing. Numerous studies have established connections between the development of ED and conditions like diabetes, hyperlipidemia, hypertension and lower urinary tract symptoms. Certain epidemiological studies have reported that ED may serve as a marker for cardiovascular disease and coronary heart disease [7,8]. While many studies have focused on the incidence rate among men over 40 years old, there has been a notable lack of attention given to the condition in younger men. Surprisingly, a recent naturalistic study showed that nearly a quarter of men seeking medical help for ED are under the age of 40 [9]. It is evident that addressing young individuals suffering from ED is imperative, highlighting the urgent need for further investigation.
3.Pathophysiology
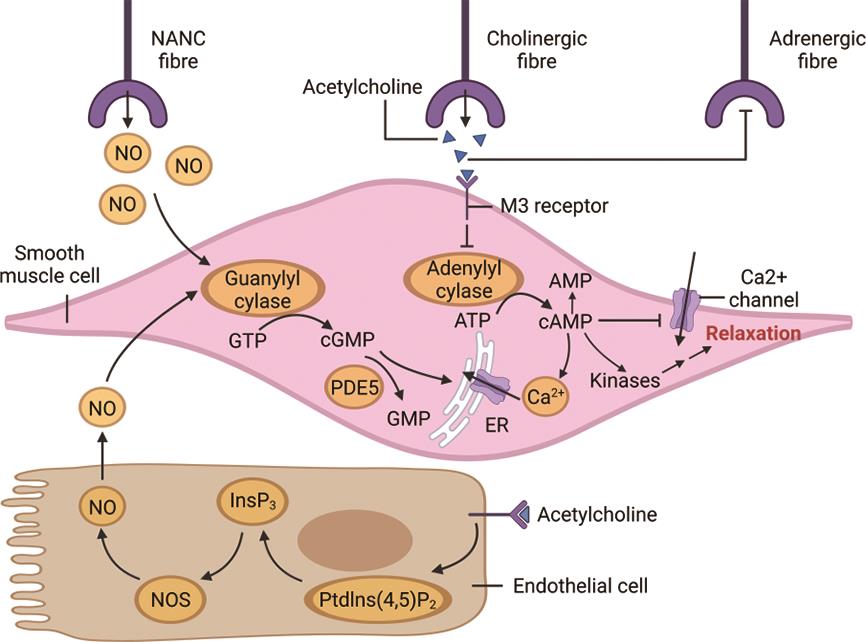
Even though penile erection may appear as a straightforward hemodynamic phenomenon, the intricate changes that occur in blood flow, intracavernosal pressure, and penile volume during the erectile process are extremely complex and necessitate precise coordination to operate effectively [10]. Normally, when the smooth muscle contracts, the penis remains in a relaxed state. Erection is primarily controlled by a spinal reflex that engages various central and peripheral neural and/or humoral mechanisms depending on the context [11]. Upon sexual stimulation, noradrenergic noncholinergic (NANC) nerve fibers release nitric oxide (NO), and parasympathetic cholinergic nerve fibers release acetylcholine. Subsequently, the regulation of NO leads to an elevation in the cyclic guanosine monophosphate (cGMP) concentration, while the presence of acetylcholine increases the cyclic adenosine monophosphate (cAMP) levels. These changes collectively inhibit extracellular Ca2+ uptake, lowering intracellular Ca2+ content, resulting in relaxation of smooth muscle cells (SMCs) (Figure 1). This relaxation permits blood to fill the lacunar spaces in the corpora cavernosa (CC). Conversely, phosphodiesterase type 5 (PDE5) catalyzes the hydrolysis of cGMP, initiating the return of the penis to the flaccid state. ED arises when any part of this processes is disrupted. In addition to the classic signaling pathway, a newly discovered mechano-regulated pathway involving YAP/TAZ signaling in SMCs has been identified to enhance male erectile function. This pathway upregulates adrenomedullin transcription, thus relaxing the SMCs to sustain erection [12]. Moreover, this mechanoregulation is independent of the aforementioned signaling pathway.
The roles of endothelial cells and SMCs in penile erection are well recognized; however, the substantial population of fibroblasts in the CC has been largely overlooked [13]. A recent study revealed that CC fibroblasts can reduce the effects of norepinephrine, impeding its vasoconstrictor function, thus promoting vasodilation and facilitating erection [14]. Furthermore, decreased Notch signaling in CC fibroblasts was associated with an increase in their abundance and improved blood flow. This novel understanding of the involvement of fibroblasts in blood flow regulation could unveil new therapeutic possibilities for ED, suggesting that restoring the fibroblast population and adjusting Notch signaling in penile fibroblasts may be beneficial for penis erection.
3.1.Psychogenic Erectile Dysfunction
Psychogenic ED, alternatively referred to as non-organic ED, is a crucial aspect to address when assessing and treating men with this condition. Stress, anxiety, and depression frequently contribute to are commonly related to the challenges in attaining and sustaining an erection before or during sexual intercourse, frequently associated with psychogenic ED [15,16]. The psychosocial determinants of ED are generally categorized into immediate and remote causes [17]. Immediate causes include performance anxiety, insufficient stimulation, and relationship conflicts, with performance anxiety recognized as a primary contributor to psychogenic ED [18]. Men experiencing performance anxiety often adopt a “spectator role”, focusing their attention predominantly on sexual performance rather than on erotic stimulation [19]. Moreover, among the remote causes, various studies hive emphasized the impact of childhood sexual trauma, issues related to sexual identity, unresolved partner conflicts, and religious or cultural taboos [20]. A web-based survey involving 844 North American medical students, with an average age of 25.7 years, reported a 13% prevalence of ED and highlighted a significant correlation between ED and depressive symptoms [21].
3.2.Organic Erectile Dysfunction
3.2.1.Neurogenic Erectile Dysfunction
Neurogenic ED is characterized by the inability to achieve and uphold a penile erection due to neurologic dysfunction, which can stem from central or peripheral neuropathies or traumatic neural loss. Common triggers encompass stroke, spinal cord injuries, traumatic brain injuries, multiple sclerosis, Parkinson’s disease, lumbar disc disease, and radical pelvic surgeries [22]. Among neurologic dysfunctions, upper motor neuron lesions can impede the central nervous system’s (CNS) control over erection. Conversely, sacral lesions induce structural and functional alterations due to the reduced innervation. Structural changes primarily involve apoptosis of the SMCs and endothelial cells in blood vessels. while the functional aspect entails a decline in NO availability in SMCs.
3.2.2.Vasculogenic Erectile Dysfunction
Penile erection is fundamentally dependent on vascular mechanisms, with vasculogenic ED being the predominant cause of organic ED. This condition results from impairment of endothelial-dependent or independent smooth muscle relaxation, contributing to functional vascular ED in its initial stages, or the occlusion of the cavernosal arteries by atherosclerosis, leading to late-stage structural vascular ED, or a combination of both [23]. Additionally, vasculogenic ED may occur as a result of venous occlusion dysfunction (VOD), defined as the erectile chamber’s inability to retain an adequate volume of blood for physiological functions. VOD is particularly prevalent among elderly patients and is often linked to conditions such as diabetes, radical prostatectomy, and androgen deprivation therapy [24,25]. Insufficient venous outlet occlusion is considered the primary cause of VOD [26]. Given its common pathophysiological foundation, vasculogenic ED can indicate an underlying vascular disorder. For instance, in the context of cardiovascular disease, in cases of a given atherosclerotic burden, the narrower penile arteries tend to obstruct earlier than the larger coronary arteries [27]. Moreover, due to the larger endothelial surface area of the smaller penile arteries, a more substantial vasodilatory response is needed for erection to occur. Consequently, ED can serve as a predictor of the risk of future fatal and non-fatal cardiovascular events.
3.2.3.Drug-Induced Erectile Dysfunction
Certain surgeries can result in iatrogenic ED, with radical pelvic surgery being the most prevalent cause. Typically, the damage during these procedures is mainly neurogenic; however, an accessory pudendal artery lesion can also contribute to the development of ED [28]. In addition, various medications have been linked to ED development. Drugs used for hypertension, including thiazide diuretics and β-blockers, digoxin, antidepressant drugs, and opiates, have all demonstrated associations with ED [29] (Table 1).
Potential Mechanisms of Drug-Induced ED.
| Drug | Potential Mechanism |
|---|---|
| Thiazide diuretics | Can cause hypovolemia and hypotension, electrolyte imbalance, reduced production of testosterone and increased production of prolactin, dehydration and activation of the renin–angiotensin–aldosterone system. [30–32]. |
| β-blockers | Reduced cardiac output, blood flow, and oxygen delivery to the penis, along with the blockade of β-adrenergic receptors on the penile smooth muscle and nerves, can cause or aggravate ED [30,33]. However, a newer agent called nebivolol may improve ED by increasing the generation of NO [34]. |
| Digoxin | Affects plasma testosterone levels and lead to a significant decrease in sexual desire, erection quality and the frequency of sexual relations [35]. |
| Serotonin/norepinephrine reuptake inhibitors (SNRIs) | Affects erection through its interaction with α-2 adrenergic receptors, which play a role in the contraction of CC SMCs [36]. Additionally, serotonin acts as an endogenous contractile agent that also promotes erection [37]. This is why SNRIs can significantly increase the incidence of ED [38,39]. |
| Selective serotonin reuptake inhibitor (SSRI) | SSRI may lead to alterations in libido and ED through direct and indirect effects on various neurotransmitters, including serotonin, dopamine, and norepinephrine [40,41]. |
3.2.4.Endocrinological Erectile Dysfunction
Androgens are considered as the primary hormonal regulator for penile development and physiology [42]. While a portion of the erectile response to testosterone is mediated through sexual desire (as testosterone influences the male sex drive) [43], studies have revealed direct effects of testosterone on CC SMCs [44]. Moreover, there is evidence supporting the role of androgen in erectile function, with a defined threshold of 200 ng/dL of testosterone for routine nocturnal erections [45]. Additionally, studies have shown a correlation between thyroid dysfunction and ED, indicating that a deficiency in thyroid hormones can contribute to the condition [46]. Subsequent research has indicated that hypothyroidism may be associated with decreased levels of serum testosterone, dehydroepiandrosterone, and dehydroepiandrosterone sulfate, ultimately leading to ED by reducing the testosterone bioavailability. In addition to androgens, hyperprolactinemia also results in a decrease in sexual desire, which may consequently contribute to the development of ED [47]. Moreover, while endocrine causes can lead to ED, it can also serve as an early marker of endocrine and glycemic disorders [48].
3.2.5.Metabolic Causes
Metabolic factors such as metabolic syndrome (MetS)—a clustering of medical conditions including hyperglycemia, hypertension, dyslipidemia, and abdominal obesity—are recognized risk factors for ED [49]. The association between MetS and ED has been evident since the early 21st century [50,51]. Two meta-analyses of observational studies demonstrated that the presence of MetS increases the risk of ED by a factor ranging from 1.6 to 2.6. Furthermore, nearly all components defining the MetS construct independently elevate the odds of developing ED, with the exception of HDL-cholesterol reduction [52,53]. Given that MetS is frequently associated with decreased testosterone levels [54] and that testosterone levels are closely linked to male sexual function [55], it is plausible that MetS-related testosterone deficiency may contribute to the onset of ED.
3.2.6.Inflammatory/Infectious Causes
Inflammatory cytokines (ICs) play a crucial role in ED, and alterations in ICs levels significantly influence the risk of developing ED [56]. For instance, male accessory gland infection/inflammation (MAGI) serves as a comprehensive term encompassing a spectrum of inflammatory diseases affecting the male accessory sexual glands. Studies have indicated a higher prevalence of ED among patients with MAGI compared to the general population [57]. The pathogenesis of ED in this context may involve several interconnected pathways, initiated by stimuli such as infection and dysfunctional urinary flow, which can lead to neuropathic conditions affecting the pelvic nerves, muscles and the prostatic tissue.
3.2.7.Mechanical Causes
Experimental evidence has demonstrated that the mechano-regulated YAP/TAZ signaling in SMCs plays a crucial role in ED and penile rehabilitation [12]. For instance, induratio penis plastica (IPP) can affects the connective tissue layer surrounding the CC, known as the tunica albuginea, leading to plaque formation, loss of tissue elasticity, and deformation of the penis, ultimately contributing to the development of ED [58].
4.Diagnosis
The primary basis for diagnosing ED is a thorough and comprehensive medical and sexual history. During the initial visit, the primary care physician should endeavor to obtain a detailed psychosocial history, with a particular emphasis on the patient’s self-assessment of sexual performance and his general attitudes and knowledge regarding sexuality. Interviewing the patient’s partner during the ED assessment can also be beneficial.
Standardized questionnaires are frequently employed to confirm the diagnosis of true ED and evaluate its severity. These questionnaires serve as valuable research tools that assess response to various treatments. One of the most practical and easily administered is the five-item International Index of Erectile Function (IIEF-5) questionnaire [59,60]. The severity of ED is typically classified as mild, moderate or severe based on the IIEF-5 scores: a score of 1 to 7 indicates severe, 8 to 11 indicates moderate, 12 to 16 indicates mild–moderate, 17 to 21 indicates mild, and 22 to 25 indicates the absence of ED.
Furthermore, numerous specific investigations exist for diagnosing of ED. Color doppler ultrasound can be used alongside a historical gold standard, pharmaco-arteriography, to diagnose arteriogenic ED and may also suggest other vascular issues, such as coronary artery disease. Pharmaco-cavernosometry or cavernosography is used to identify venogenic ED and delineates the site of leak and cavernosal abnormalities. Neurological testing assesses somatic pathways, while nocturnal penile tumescence testing is considered the closest to a gold standard for differentiating between psychogenic from organic ED [61].
5.Management
5.1.Lifestyle Modification
Numerous studies have established a clear link between ED and unhealthy lifestyle factors such as smoking, obesity, and sedentary behavior. Therefore, lifestyle modifications play a crucial role in improving this condition, particularly among younger patients. A meta-analysis involving four prospective cohort studies and four case-control studies, encompassing 28,586 participants, suggested that the overall odds ratio of ED was 1.51 for current smokers and 1.29 for former smokers when compared to non-smokers [62]. Moreover, another study demonstrated a remarkable enhancement in erectile capacity within just one day of smoking cessation, highlighting the vital role of quitting smoking in restoring erectile function [63]. In addition, a 2011 meta-analysis of six randomized controlled trials, comprising 740 participants, assessed the impact of lifestyle changes on the severity of ED [64]. Their findings suggested that weight loss and increased physical activity could enhance erectile function by improving insulin resistance, endothelial dysfunction, and low-grade inflammation associated with diabetes and metabolic disorders, all of which are common risk factors for ED. The available data support recommendations advocating dietary improvements and physical activity in obese men to achieve weight loss, while emphasizing that all adult men engage in at least 30 min of moderate-intensity aerobic exercise most days of the week [65].
5.2.Medical Therapy
5.2.1.Phosphodiesterase Inhibitors
Phosphodiesterases (PDE) constitute a diverse group of esterases responsible for hydrolysis of cyclic nucleotides [66]. This enzymatic breakdown mainly occurs within the vascular SMCs of the CC. The enzyme comprises two subunits--a catalytic domain and an allosteric domain. cGMP, essential for muscle relaxation and erection, binds to the catalytic domain, subsequently leading to linear formation of 5′-GMP post-hydrolysis [67]. Consequently, the reduction in cGMP levels inhibits erection. Inhibitors targeting this enzyme function by preventing cGMP degradation, thereby elevating its concentration to promote erectile function.
PDE5 inhibitors (PDE5-Is) are recommended as the first-line treatment according to current guidelines for ED. Sildenafil, tadalafil, and vardenafil are notable for their safety and efficacy among PDE5-Is. Currently, four PDE5-Is, specifically sildenafil, tadalafil, vardenafil and avanafil, are available globally, while mirodenafil, udenafil and lodenafil are restricted to certain countries. The medications come in various formulations, including pills and films, each with specific dosages. Although the mechanism of action is similar across all PDE-Is, their pharmacokinetic properties differ. Clinical evaluations during exercise testing in patients with coronary artery disease (CAD) or heart failure revealed that PDE5-Is do not increase the risk of myocardial infarction, mortality, or worsen ischemia or cardiac hemodynamics [68]. However, the simultaneous use of PDE5-Is and nitrates is contraindicated due to the heightened risk of severe hypotension [67]. Common side effects of PDE5-Is are typically mild and well-tolerated, with headache being predominant, followed by flushing. While sildenafil may lead to indigestion and occasional visual disturbances [69], tadalafil may cause back pain and myalgia. The overall response rate of PDE5-Is ranges between 60 to 70%; however, certain patient groups, including those with severe nerve damage, post-radical prostatectomy ED, diabetes, or severe vascular disease, often display significantly reduced response rates. The ineffectiveness of PDE5-Is may be attributed to the fact that some causes of ED involve novel signaling pathways rather than conventional issues associated with PDE5 [28,70]. New drugs targeted towards patients unresponsive to PDE5-Is are also under development [71].
5.2.2.Testosterone
Testosterone replacement therapy (TRT) is recommended for individuals with low bioavailable testosterone levels. The main goal of TRT is to raise testosterone levels to the mid-normal range to mimic natural endogenous production while minimizing adverse effects and safety concerns [72]. A meta-analysis of 16 studies demonstrated that male hypogonadism patients treated with testosterone experienced more pronounced improvements in ED compared to those receiving a placebo [73]. Additionally, for elder men with deficient testosterone concentrations who do not exhibit an initial response to PDE5-Is, testosterone is utilized in combination with PDE5-Is as part of treatment regimen [71,74].
5.2.3.Organic Nitrates
Nitroglycerin and other organic nitrates are known to induce smooth muscle relaxation by activating soluble guanylate cyclase through enzymatic hydrolysis of NO, providing a plausible mechanism to enhance erectile function in men with ED. The observation that topical application of nitroglycerin to the penis can lead to a satisfactory erection for sexual intercourse has sparked numerous investigations into the efficacy of this potential approach for treating ED. Although the effectiveness transdermal nitroglycerin has been established in several placebo-controlled studies, its impact is limited, rendering this treatment option nonviable currently, notably due to contraindication of organic nitrates for individuals taking PDE5-Is.
5.2.4.Alpha-Adrenoceptor Antagonists
The sympathetic nervous system induces CC smooth muscle contraction by releasing noradrenaline (NA) and stimulating alpha-adrenoceptors (ARs), a process closely linked to ED development. Antagonizing α-AR appears to be a promising approach to ED treatment, although therapeutic outcomes remain somewhat constrained. Research has indicated that phentolamine promotes penile erection by blocking α1 and α2 ARs, potentially involving activation of NO synthase [75]. Initial studies have demonstrated some efficacy of oral or buccal phentolamine in patients with non-specific ED [76,77]. Additionally, at the necessary dose range (20–40 mg) to boost erectile response, minimal adverse cardiovascular effects have been noted [78]. Yohimbine, another ɑ-AR antagonist, selectively targets α2-ARs. The primary site of action of yohimbine is likely within the CNS, as the intracavernosal injection of idazoxan, a more potent α2-AR antagonist, failed to induce penile erection [79]. Yohimbines’s efficacy in men with organic ED was confirmed, with a 43% response rate compared to 28% for the placebo [80]. Similar response rates were observed in studies using the same design for individuals with psychogenic ED [81].
5.2.5.Chinese Herbs
Chinese herbs serve as an effective alternative therapy aimed at enhancing the therapeutic effect for ED. To date, numerous traditional Chinese herbs have been utilized for the treatment of ED, either alone or in combination within formulated compounds. For instance, the potential mechanism of Semen cuscutae in treating ED may involve increasing testosterone levels [82]. Additionally, Ligusticum chuanxiong Hort is believed to elevate the concerntrations of cAMP and cGMP [83]. Furthermore, Folium Ginkgo Bilobae may enhance the expression of neural nitric oxide synthase (nNOS) and boost dopaminergic activity [84–86].
5.2.6.Physical Therapy
Vacuum Erection Devices
Vacuum erection devices (VED) are mechanical devices placed over the penis to generate a negative pressure vacuum that facilitates the influx of blood into the penile tissues through manual pumping [87]. This process induces engorgement of the lacunar spaces within the CC, leading to tumescence. Typically, this device is complemented by a constriction band positioned at the base of the penis to prevent the backflow of blood post-tumescence. In a 1991 study, it was found that 75% of diabetic men with ED were able to engage in sexual intercourse by employing a VED to achieve tumescence [88]. Nevertheless, the resulting erections from this method are often perceived as artificial and mechanized, possibly causing a cold sensation in the penis, leading to dissatisfaction among around half of the patients. Furthermore, VEDs may induce adverse effects such as penile numbness, petechiae, and delayed ejaculation.
Prostaglandin E1 Injection
Prostaglandins exhibit significant therapeutic efficacy for ED. In contrast to PDE5-Is, this drug category exerts a direct mechanism of action. When prostaglandin E1 (PGE1) binds to its receptors, it activates the cyclic adenosine monophosphate pathway, resulting in SMC relaxation [89]. Furthermore, this process also stimulates protein kinase A, promoting SMC relaxation by inhibiting potassium and calcium flow within the cell. Prostaglandins can be administered through intracorporal injection or topically/percutaneously. Patients treated with PGE1 intracorporal injection therapy have shown promising outcomes, particularly for those unresponsive to oral medications. Research indicated that PGE1 induced a sufficiently rigid erection for sexual activity in 72.6% of ED patients [90–92]. However, the use of PGE1 often injections frequently lead to penile pain, and bruising is a common occurrence.
5.2.7.Low-Intensity Extracorporeal Shock Wave Therapy
Extracorporeal shock wave (ESW) employs two-way sound waves to transmit energy, with clinical applications varying according to the energy density levels [93]. Notably, low-energy density ESW is recognized for its ability to promote angiogenesis and improve blood supply, rendering it effective for the treatment of chronic injuries, musculoskeletal recovery, and cardiovascular disease [94,95]. Research has identified a significant mechanism underlying ED as the impairment or injury to vascular endothelial function [96,97]. Low-intensity extracorporeal shock wave therapy (LI-ESWT) has demonstrated its capacity to stimulate the expression of angiogenesis-related factors, such as vascular endothelial growth factor (VEGF), thereby promoting vascular regeneration [98–100]. Consequently, LI-ESWT has gained increasing traction in the clinical management of ED [101,102].
Acupuncture
Acupuncture, defined as the insertion of needles into specific acupoints located in the skin and underlying tissues, represents a significant therapeutic modality for various diseases in traditional Chinese medicine (TCM). It is posited that the neurophysiological effects of acupuncture arise from the activation of the central nervous system and the modulation of neurotransmitters [103]. Furthermore, acupuncture may play a role in regulating the release of NO and certain neuropeptides involved in the erection process [104]. Findings from a study suggest that acupuncture is an effective intervention for psychogenic ED, with a patient satisfaction rate of 68.4% in the treatment group, significantly surpassing that of the placebo group [103].
5.2.8.Stem Cell Therapy
Stem cells are defined as undifferentiated or partially differentiated cells, characterized by their ability to self-renew and differentiate into more specialized cell types [105]. In recent years, stem cell therapy has been emerged as a potential treatment for ED due to the capacity of stem cells to differentiate into endothelial, neuronal or smooth muscle cells, thereby restoring structural damage that may occur in the penile tissues of ED patients. The stem cells utilized in preclinical studies on ED primarily include bone marrow-derived stem cells (BMSCs) [106], adipose tissue-derived stem cells (ADSCs) [107], embryonic stem cells (ESCs) [105], and muscle-derived (MDSCs) [108]. Moreover, encouraging results have been reported from clinical studies utilizing stem cells [109–112].
Penile Prosthesis Implantation
Penile prosthesis implantation, recognized as a third-line treatment for ED, stands out as a successful surgical intervention utilized for ED treatment since 1973 [113]. Typically, this procedure is reserved for patients who have not responded to other treatment options. The hydraulic three-piece implant currently leads as the most favored penile prosthesis, replicating the natural erection process by transitioning between erect and flaccid states. Studies have demonstrated that over 90% of individuals with penile implants achieve successful sexual intercourse with their partners [114]. Despite its effectiveness, penile prosthesis implantation is associated with traumatic cost and potential for rare yet severe complications, such as prosthesis infection and pump migration, necessitating further surgical procedures or interventions. To address these challenges, novel methods are being developed to prevent the occurrence of complications [115].
6.Conclusions
ED is a disease is a chronic medical condition with substantial implications for men’s well-being. The introduction of PDE5-Is around three decades ago marked a pivotal advancement in ED treatment, establishing these drugs as the primary approach globally. Nevertheless, it has become evident that not all individuals with ED respond favorably to PDE5-Is, with some cases exhibiting complete ineffectiveness. Studies indicate that failures with PDE5-Is commonly arise in instances of compromised vascular and neural supply to the CC smooth muscles, often seen in conditions like hypertension, diabetes, atherosclerosis, and dyslipidemia, as well as following pelvic surgery, prostatectomy, and penile trauma. These conditions typically lead to substantial alterations in the morphology, physiology and neurophysiology of various penile tissues. The precise mechanism underlying the development of PDE5-Is resistance in many patients remains incompletely understood, promoting ongoing exploration of various pharmacological strategies to address this challenge.
Several studies have explored alternative therapies beyond PDE5-Is. Evidence indicates that multimodal therapy yields beneficial long-term effects in reducing ED symptoms, particularly through the combined use of tadalafil and LI-ESWT [116]. LI-ESWT has emerged as a viable treatment option for patients with severe ED who demonstrate inadequate or no response to PDE5-Is, with its advantages being independent of the NO and cGMP pathways [117]. Consequently, a synergistic effect between LI-ESWT and PDE5-Is has been observed. Studies have shown that a combined approach involving 5 mg of tadalafil taken once daily and a LI-ESWT protocol using 2400 shockwaves demonstrates significant therapeutic effect [118].
However, the outlined treatment strategies have shown limited progress in overcoming PDE5-Is failures in the management of ED thus far. Most drugs derived from experimental strategies primarily affect systemic blood pressure, posing challenges in compatibility with ED therapy. Despite considerable experimental research in animal models and numerous clinical studies, few studies have involved human tissue- and cell-based mechanisms, and even fewer drugs have progressed to clinical trials. Looking ahead, more advanced and effective strategies may be necessary for ED, such as stem-cell therapy and gene-transfer-based interventions. Furthermore, the discovery of innovative drugs targeting novel pathways could offer valuable assistance for managing complex or refractory cases of ED.
Recent research has shown a rising interest in nutraceuticals, defined as bioactive compounds derived from natural sources, including vitamins, minerals, herbs, and other dietary supplements. Certain nutraceuticals have demonstrated the capacity to modulate various physiological pathways that influence erectile function. Studies have indicated that several nutraceutical agents, such as alkaloid, polyphenols, and amino acids, may exhibit PDE5 inhibitory effects, thereby facilitating the release of NO, increasing cGMP levels, and promoting the relaxation of penile smooth muscles—all of which are critical for the achievement and maintenance of erections [119,120].
ED not only affects man’s sexual function but also his psychological well-being. It can lead to depression and anxiety, impacting both individual and their partner’s sexual satisfaction and overall relationship quality. Furthermore, ED can serve as an early indicator of systemic endothelial dysfunction predicting cardiovascular health and potential silent myocardial ischemia. Despite advancements in comprehending erection physiology and ED pathophysiology, the urgent need for more efficacious therapeutic medications capable of delivering lasting relief for erectile dysfunction persists.
Author Contributions: S. W.: writing—original draft preparation, writing—reviewing and editing; H. L.: conceptualization; Y. Z.: conceptualization, supervision; Y. L.: supervision, writing—reviewing and editing. All authors have read and agreed to the published version of the manuscript.
Funding: This research was funded by National Key R&D Program of China (2021YFF05014041 and 2018YFA0800501 to Y. Z., 2021YFF0501404 to Y. L.); National Science Foundation of China (82325004 and 92168114 to Y. Z., 82170422 to Y. L., 82371633 to H. L.); Beijing Municipal Natural Science Foundation (7232096 to Y. L., F251013 to Y. Z., 72121134 to H. L.); Research Project of Peking University in State Key Laboratory of Vascular Homeostasis and Remodeling (Peking University) to Y. Z.; Peking University Clinical Scientist Training Program and the Fundamental Research Funds for the Central University (BMU2023PYJH012) to H. L..
Institutional Review Board Statement: Not applicable.
Informed Consent Statement: Not applicable.
Data Availability Statement: Not applicable.
Conflicts of Interest: The authors declare no potential conflict of interest.
References
- 1.
McCabe, M.P; Sharlip, I.D; Atalla, E; et al. Definitions of Sexual Dysfunctions in Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. J. Sex. Med. 2016, 13, 135–143. https://doi.org/10.1016/j.jsxm.2015.12.019.
- 2.
Yafi, F.A; Jenkins, L; Albersen, M; et al. Erectile dysfunction. Nat. Rev. Dis. Primers 2016, 2, 16003. https://doi.org/10.1038/nrdp.2016.3.
- 3.
WHO. Developing Sexual Health Programmes. Available online: https://www.who.int/publications/i/item/WHO-RHR-HRP-10.22.(accessed on 29 July 2024).
- 4.
Mark, K.P; Arenella, K; Girard, A; et al. Erectile dysfunction prevalence in the United States: Report from the 2021 National Survey of Sexual Wellbeing. J. Sex. Med. 2024, 21, 296–303. https://doi.org/10.1093/jsxmed/qdae008.
- 5.
Muneer, A; Kalsi, J; Nazareth, I; et al. Erectile dysfunction. BMJ 2014, 348, g129. https://doi.org/10.1136/bmj.g129.
- 6.
Shamloul, R; Ghanem, H; Erectile dysfunction. Lancet 2013, 381, 153–165. https://doi.org/10.1016/s0140-6736(12)60520-0.
- 7.
Chung, S.D; Chen, Y.K; Lin, H.C; et al. Increased risk of stroke among men with erectile dysfunction: A nationwide population-based study. J. Sex. Med. 2011, 8, 240–246. https://doi.org/10.1111/j.1743-6109.2010.01973.x.
- 8.
Inman, B.A; Sauver, J.L; Jacobson, D.J; et al. A population-based, longitudinal study of erectile dysfunction and future coronary artery disease. Mayo Clin. Proc. 2009, 84, 108–113. https://doi.org/10.4065/84.2.108.
- 9.
Capogrosso, P; Colicchia, M; Ventimiglia, E; et al. One patient out of four with newly diagnosed erectile dysfunction is a young man--worrisome picture from the everyday clinical practice. J. Sex. Med. 2013, 10, 1833–1841. https://doi.org/10.1111/jsm.12179.
- 10.
Andersson, K.E; Wagner, G; Physiology of penile erection. Physiol. Rev. 1995, 75, 191–236. https://doi.org/10.1152/physrev.1995.75.1.191.
- 11.
Andersson, K.E. Mechanisms of penile erection and basis for pharmacological treatment of erectile dysfunction. Pharmacol. Rev. 2011, 63, 811–859. https://doi.org/10.1124/pr.111.004515.
- 12.
Ji, M; Chen, D; Shu, Y; et al. The role of mechano-regulated YAP/TAZ in erectile dysfunction. Nat. Commun. 2023, 14, 3758. https://doi.org/10.1038/s41467-023-39009-z.
- 13.
Fang, D; Tan, X.H; Song, W.P; et al. Single-Cell RNA Sequencing of Human Corpus Cavernosum Reveals Cellular Heterogeneity Landscapes in Erectile Dysfunction. Front. Endocrinol. 2022, 13, 874915. https://doi.org/10.3389/fendo.2022.874915.
- 14.
Guimaraes, E.L; Dias, D.O; Hau, W.F; et al. Corpora cavernosa fibroblasts mediate penile erection. Science 2024, 383, eade8064. https://doi.org/10.1126/science.ade8064.
- 15.
Jannini, E.A; Sternbach, N; Limoncin, E; et al. Health-related characteristics and unmet needs of men with erectile dysfunction: A survey in five European countries. J. Sex. Med. 2014, 11, 40–50. https://doi.org/10.1111/jsm.12344.
- 16.
Khoo, E.M; Tan, H.M; Low, W.Y; Erectile dysfunction and comorbidities in aging men: An urban cross-sectional study in Malaysia. J. Sex. Med. 2008, 5, 2925–2934. https://doi.org/10.1111/j.1743-6109.2008.00988.x.
- 17.
Laumann, E.O; Paik, A; Rosen, R.C; Sexual dysfunction in the United States: Prevalence and predictors. JAMA 1999, 281, 537–544. https://doi.org/10.1001/jama.281.6.537.
- 18.
Rosen, R.C; Leiblum, S.R; Spector, I.P; Psychologically based treatment for male erectile disorder: A cognitive-interpersonal model. J. Sex Marital. Ther. 1994, 20, 67–85. https://doi.org/10.1080/00926239408403419.
- 19.
Brecher, E.M. Human sexual inadequacy. Med. J. Aust. 1971, 1, 3–4. https://doi.org/10.5694/j.1326-5377.1971.tb87410.x.
- 20.
Mohr, D.C; Beutler, L.E; Engle, D; et al. Identification of patients at risk for nonresponse and negative outcome in psychotherapy. J. Consult. Clin. Psychol. 1990, 58, 622–628. https://doi.org/10.1037//0022-006x.58.5.622.
- 21.
Smith, J.F; Breyer, B.N; Eisenberg, M.L; et al. Sexual function and depressive symptoms among male North American medical students. J. Sex. Med. 2010, 7, 3909–3917. https://doi.org/10.1111/j.1743-6109.2010.02033.x.
- 22.
Lue, T.F. Neurogenic erectile dysfunction. Clin. Auton. Res. 2001, 11, 285–294. https://doi.org/10.1007/bf02332973.
- 23.
Vlachopoulos, C; Jackson, G; Stefanadis, C; et al. Erectile dysfunction in the cardiovascular patient. Eur. Heart J. 2013, 34, 2034–2046. https://doi.org/10.1093/eurheartj/eht112.
- 24.
Peşkircioğlu, L; Tekin, I; Boyvat, F; et al. Embolization of the deep dorsal vein for the treatment of erectile impotence due to veno-occlusive dysfunction. J. Urol. 2000, 163, 472–475. https://doi.org/10.1016/s0022-5347(05)67904-9.
- 25.
Berardinucci, D; Morales, A; Heaton, J.P; et al. Surgical treatment of penile veno-occlusive dysfunction: Is it justified? Urology 1996, 47, 88–92. https://doi.org/10.1016/s0090-4295(99)80388-4.
- 26.
Rajfer, J; Rosciszewski, A; Mehringer, M; Prevalence of corporeal venous leakage in impotent men. J. Urol. 1988, 140, 69–71. https://doi.org/10.1016/s0022-5347(17)41489-3.
- 27.
Montorsi, P; Montorsi, F; Schulman, C.C; Is erectile dysfunction the “tip of the iceberg” of a systemic vascular disorder? Eur. Urol. 2003, 44, 352–354. https://doi.org/10.1016/s0302-2838(03)00307-5.
- 28.
Tal, R; Valenzuela, R; Aviv, N; et al. Persistent erectile dysfunction following radical prostatectomy: The association between nerve-sparing status and the prevalence and chronology of venous leak. J. Sex. Med. 2009, 6, 2813–2819. https://doi.org/10.1111/j.1743-6109.2009.01437.x.
- 29.
Francis, M.E; Kusek, J.W; Nyberg, L.M; et al. The contribution of common medical conditions and drug exposures to erectile dysfunction in adult males. J. Urol. 2007, 178, 591–596; discussion 596. https://doi.org/10.1016/j.juro.2007.03.127.
- 30.
Carella, M.C; Forleo, C; Stanca, A; et al. Heart Failure and Erectile Dysfunction: A Review of the Current Evidence and Clinical Implications. Curr. Heart Fail. Rep. 2023, 20, 530–541. https://doi.org/10.1007/s11897-023-00632-y.
- 31.
Wassertheil-Smoller, S; Blaufox, M.D; Oberman, A; et al. Effect of antihypertensives on sexual function and quality of life: The TAIM Study. Ann. Intern. Med. 1991, 114, 613–620. https://doi.org/10.7326/0003-4819-114-8-613.
- 32.
Scharf, M.B; Mayleben, D.W; Comparative effects of prazosin and hydrochlorothiazide on sexual function in hypertensive men. Am. J. Med. 1989, 86, 110–112. https://doi.org/10.1016/0002-9343(89)90144-7.
- 33.
Gungor, G; Perk, H; Soyupek, S; et al. Nebivolol protects erectile functions compared to Metoprolol in hypertensive men with atherogenic, venogenic, psychogenic erectile dysfunction: A prospective, randomized, cross-over, clinical trial. Eur. J. Intern. Med. 2022, 103, 69–75. https://doi.org/10.1016/j.ejim.2022.06.013.
- 34.
Viigimaa, M; Vlachopoulos, C; Lazaridis, A; et al. Management of erectile dysfunction in hypertension: Tips and tricks. World J. Cardiol. 2014, 6, 908–915. https://doi.org/10.4330/wjc.v6.i9.908.
- 35.
Neri, A; Zukerman, Z; Aygen, M; et al. The effect of long-term administration of digoxin on plasma androgens and sexual dysfunction. J. Sex Marital. Ther. 1987, 13, 58–63. https://doi.org/10.1080/00926238708403879.
- 36.
Azadzoi, K.M; Yang, J; Siroky, M.B; Neural regulation of sexual function in men. World J. Clin. Urol. 2013, 2, 32–41. https://doi.org/10.5410/wjcu.v2.i3.32.
- 37.
Lau, D.H; Thompson, C.S; Bellringer, J.F; et al. Doxazosin and serotonin (5-HT) receptor (1A, 2A, and 4) antagonists inhibit 5-HT-mediated human cavernosal contraction. J. Androl. 2006, 27, 679–685. https://doi.org/10.2164/jandrol.106.000547.
- 38.
Trinchieri, M; Trinchieri, M; Perletti, G; et al. Erectile and Ejaculatory Dysfunction Associated with Use of Psychotropic Drugs: A Systematic Review. J. Sex. Med. 2021, 18, 1354–1363. https://doi.org/10.1016/j.jsxm.2021.05.016.
- 39.
Mazzilli, R; Angeletti, G; Olana, S; et al. Erectile dysfunction in patients taking psychotropic drugs and treated with phosphodiesterase-5 inhibitors. Arch. Ital. Di Urol. Androl. 2018, 90, 44–48. https://doi.org/10.4081/aiua.2018.1.44.
- 40.
Williams, V.S; Edin, H.M; Hogue, S.L; et al. Prevalence and impact of antidepressant-associated sexual dysfunction in three European countries: Replication in a cross-sectional patient survey. J. Psychopharmacol. 2010, 24, 489–496. https://doi.org/10.1177/0269881109102779.
- 41.
Clayton, A.H; Croft, H.A; Handiwala, L; Antidepressants and sexual dysfunction: Mechanisms and clinical implications. Postgrad. Med. 2014, 126, 91–99. https://doi.org/10.3810/pgm.2014.03.2744.
- 42.
Baskin, L.S; Sutherland, R.S; DiSandro, M.J; et al. The effect of testosterone on androgen receptors and human penile growth. J. Urol. 1997, 158, 1113–1118. https://doi.org/10.1097/00005392-199709000-00108.
- 43.
Vignozzi, L; Corona, G; Petrone, L; et al. Testosterone and sexual activity. J. Endocrinol. Investig. 2005, 28, 39–44.
- 44.
Okumu, L.A; Braden, T.D; Vail, K; et al. Low androgen induced penile maldevelopment involves altered gene expression of biomarkers of smooth muscle differentiation and a key enzyme regulating cavernous smooth muscle cell tone. J. Urol. 2014, 192, 267–273. https://doi.org/10.1016/j.juro.2013.11.101.
- 45.
Granata, A.R; Rochira, V; Lerchl, A; et al. Relationship between sleep-related erections and testosterone levels in men. J. Androl. 1997, 18, 522–527.
- 46.
Meikle, A.W. The interrelationships between thyroid dysfunction and hypogonadism in men and boys. Thyroid 2004, 14, S17–S25. https://doi.org/10.1089/105072504323024552.
- 47.
Corona, G; Rastrelli, G; Bianchi, N; et al. Hyperprolactinemia and male sexual function: Focus on erectile dysfunction and sexual desire. Int. J. Impot. Res. 2024, 36, 324–332. https://doi.org/10.1038/s41443-023-00717-1.
- 48.
Mazzilli, R; Zamponi, V; Olana, S; et al. Erectile dysfunction as a marker of endocrine and glycemic disorders. J. Endocrinol. Investig. 2022, 45, 1527–1534. https://doi.org/10.1007/s40618-022-01788-5.
- 49.
Corona, D.G; Vena, W; Pizzocaro, A; et al. Metabolic syndrome and erectile dysfunction: A systematic review and meta-analysis study. J. Endocrinol. Investig. 2023, 46, 2195–2211. https://doi.org/10.1007/s40618-023-02136-x.
- 50.
Esposito, K; Giugliano, F; Martedì, E; et al. High proportions of erectile dysfunction in men with the metabolic syndrome. Diabetes Care 2005, 28, 1201–1203. https://doi.org/10.2337/diacare.28.5.1201.
- 51.
Demir, T; Demir, O; Kefi, A; et al. Prevalence of erectile dysfunction in patients with metabolic syndrome. Int. J. Urol. 2006, 13, 385–388. https://doi.org/10.1111/j.1442-2042.2006.01310.x.
- 52.
Liu, L.H; Zhang, T; Zhang, Y.R; et al. Metabolic syndrome and risk for ED: A meta-analysis. Int. J. Impot. Res. 2014, 26, 196–200. https://doi.org/10.1038/ijir.2014.3.
- 53.
Besiroglu, H; Otunctemur, A; Ozbek, E; The relationship between metabolic syndrome, its components, and erectile dysfunction: A systematic review and a meta-analysis of observational studies. J. Sex. Med. 2015, 12, 1309–1318. https://doi.org/10.1111/jsm.12885.
- 54.
Corona, G; Monami, M; Rastrelli, G; et al. Testosterone and metabolic syndrome: A meta-analysis study. J. Sex. Med. 2011, 8, 272–283. https://doi.org/10.1111/j.1743-6109.2010.01991.x.
- 55.
Rastrelli, G; Corona, G; Maggi, M; Testosterone and sexual function in men. Maturitas 2018, 112, 46–52. https://doi.org/10.1016/j.maturitas.2018.04.004.
- 56.
Liu, D; Qin, Z; Yi, B; et al. Inflammatory cytokine profiles in erectile dysfunction: A bidirectional Mendelian randomization. Front. Immunol. 2024, 15, 1342658. https://doi.org/10.3389/fimmu.2024.1342658.
- 57.
Liang, C.Z; Zhang, X.J; Hao, Z.Y; et al. Prevalence of sexual dysfunction in Chinese men with chronic prostatitis. BJU Int. 2004, 93, 568–570. https://doi.org/10.1111/j.1464-410x.2003.04662.x.
- 58.
Sokol’shchik, M.M; Gagarina, S.V; Petrovich, R; et al. Treatment of erectile dysfunction in patients with plastic induration of the penis. Urologiia 2008, 1, 41–44.
- 59.
Rosen, R.C; Cappelleri, J.C; Smith, M.D; et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int. J. Impot. Res. 1999, 11, 319–326. https://doi.org/10.1038/sj.ijir.3900472.
- 60.
Rosen, R.C; Riley, A; Wagner, G; et al. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology 1997, 49, 822–830. https://doi.org/10.1016/s0090-4295(97)00238-0.
- 61.
Agnihotri, K; Ting, E; Francis, I.C; Current diagnosis and management of erectile dysfunction. Med. J. Aust. 2020, 212, 95–95.e1. https://doi.org/10.5694/mja2.50450.
- 62.
Cao, S; Yin, X; Wang, Y; et al. Smoking and risk of erectile dysfunction: Systematic review of observational studies with meta-analysis. PLoS ONE 2013, 8, e60443. https://doi.org/10.1371/journal.pone.0060443.
- 63.
Guay, A.T; Perez, J.B; Heatley, G.J; Cessation of smoking rapidly decreases erectile dysfunction. Endocr. Pract. 1998, 4, 23–26. https://doi.org/10.4158/ep.4.1.23.
- 64.
Gupta, B.P; Murad, M.H; Clifton, M.M; et al. The effect of lifestyle modification and cardiovascular risk factor reduction on erectile dysfunction: A systematic review and meta-analysis. Arch. Intern. Med. 2011, 171, 1797–1803. https://doi.org/10.1001/archinternmed.2011.440.
- 65.
Esposito, K; Giugliano, F; De Sio, M; et al. Dietary factors in erectile dysfunction. Int. J. Impot. Res. 2006, 18, 370–374. https://doi.org/10.1038/sj.ijir.3901438.
- 66.
Boswell-Smith, V; Spina, D; Page, C.P; Phosphodiesterase inhibitors. Br. J. Pharmaco.l 2006, 147, S252–257. https://doi.org/10.1038/sj.bjp.0706495.
- 67.
Eardley, I; Donatucci, C; Corbin, J; et al. Pharmacotherapy for erectile dysfunction. J. Sex. Med. 2010, 7, 524–540. https://doi.org/10.1111/j.1743-6109.2009.01627.x.
- 68.
Morganroth, J; Ilson, B.E; Shaddinger, B.C; et al. Evaluation of vardenafil and sildenafil on cardiac repolarization. Am. J. Cardiol. 2004, 93, 1378–1383. https://doi.org/10.1016/j.amjcard.2004.02.034.
- 69.
McGwin, G., Jr. Phosphodiesterase type 5 inhibitor use and hearing impairment. Arch.Otolaryngol. Head Neck Surg. 2010, 136, 488–492. https://doi.org/10.1001/archoto.2010.51.
- 70.
Zhao, W; Sun, J; Yao, L.Y; et al. MYPT1 reduction is a pathogenic factor of erectile dysfunction. Commun. Biol. 2022, 5, 744. https://doi.org/10.1038/s42003-022-03716-y.
- 71.
Shabsigh, R; Kaufman, J.M; Steidle, C; et al. Randomized study of testosterone gel as adjunctive therapy to sildenafil in hypogonadal men with erectile dysfunction who do not respond to sildenafil alone. J. Urol. 2004, 172, 658–663. https://doi.org/10.1097/01.ju.0000132389.97804.d7.
- 72.
Dean, J.D; McMahon, C.G; Guay, A.T; et al. The International Society for Sexual Medicine’s Process of Care for the Assessment and Management of Testosterone Deficiency in Adult Men. J. Sex. Med. 2015, 12, 1660–1686. https://doi.org/10.1111/jsm.12952.
- 73.
Jain, P; Rademaker, A.W; McVary, K.T; Testosterone supplementation for erectile dysfunction: Results of a meta-analysis. J. Urol. 2000, 164, 371–375.
- 74.
Shamloul, R; Ghanem, H; Fahmy, I; et al. Testosterone therapy can enhance erectile function response to sildenafil in patients with PADAM: A pilot study. J. Sex. Med. 2005, 2, 559–564. https://doi.org/10.1111/j.1743-6109.2005.00071.x.
- 75.
Traish, A; Gupta, S; Gallant, C; et al. Phentolamine mesylate relaxes penile corpus cavernosum tissue by adrenergic and non-adrenergic mechanisms. Int. J. Impot. Res. 1998, 10, 215–223. https://doi.org/10.1038/sj.ijir.3900351.
- 76.
Gwinup, G. Oral phentolamine in nonspecific erectile insufficiency. Ann. Intern. Med. 1988, 109, 162–163. https://doi.org/10.7326/0003-4819-109-2-162.
- 77.
Zorgniotti, A.W. Experience with buccal phentolamine mesylate for impotence. Int. J. Impot. Res. 1994, 6, 37–41.
- 78.
Davis, B.J; Chapple, C.R; Sellers, D.J; et al. α(1L)-adrenoceptors mediate contraction of human erectile tissue. J. Pharmacol. Sci. 2018, 137, 366–371. https://doi.org/10.1016/j.jphs.2018.08.003.
- 79.
Brindley, G.S. Pilot experiments on the actions of drugs injected into the human corpus cavernosum penis. Br. J. Pharmacol. 1986, 87, 495–500. https://doi.org/10.1111/j.1476-5381.1986.tb10191.x.
- 80.
Price, L.H; Charney, D.S; Heninger, G.R; Three cases of manic symptoms following yohimbine administration. Am. J. Psychiatry 1984, 141, 1267–1268. https://doi.org/10.1176/ajp.141.10.1267.
- 81.
Reid, K; Surridge, D.H; Morales, A; et al. Double-blind trial of yohimbine in treatment of psychogenic impotence. Lancet 1987, 2, 421–423. https://doi.org/10.1016/s0140-6736(87)90958-5.
- 82.
Yang, J; Wang, Y; Bao, Y; et al. The total flavones from Semen cuscutae reverse the reduction of testosterone level and the expression of androgen receptor gene in kidney-yang deficient mice. J. Ethnopharmacol. 2008, 119, 166–171. https://doi.org/10.1016/j.jep.2008.06.027.
- 83.
Xiao, H.J; Wang, T; Chen, J; et al. Chuanxiongzine relaxes isolated corpus cavernosum strips and raises intracavernous pressure in rabbits. Int. J. Impot. Res. 2010, 22, 120–126. https://doi.org/10.1038/ijir.2009.53.
- 84.
Wu, Y.N; Liao, C.H; Chen, K.C; et al. Effect of Ginkgo biloba Extract (EGb-761) on Recovery of Erectile Dysfunction in Bilateral Cavernous Nerve Injury Rat Model. Urology 2015, 85, 1214.e7–1214.e15. https://doi.org/10.1016/j.urology.2015.01.026.
- 85.
Yeh, K.Y; Wu, C.H; Tai, M.Y; et al. Ginkgo biloba extract enhances noncontact erection in rats: The role of dopamine in the paraventricular nucleus and the mesolimbic system. Neuroscience 2011, 189, 199–206. https://doi.org/10.1016/j.neuroscience.2011.05.025.
- 86.
Yeh, K.Y; Liu, Y.Z; Tai, M.Y; et al. Ginkgo biloba extract treatment increases noncontact erections and central dopamine levels in rats: Role of the bed nucleus of the stria terminalis and the medial preoptic area. Psychopharmacology 2010, 210, 585–590. https://doi.org/10.1007/s00213-010-1861-4.
- 87.
Bosshardt, R.J; Farwerk, R; Sikora, R; et al. Objective measurement of the effectiveness, therapeutic success and dynamic mechanisms of the vacuum device. Br. J. Urol. 1995, 75, 786–791. https://doi.org/10.1111/j.1464-410x.1995.tb07392.x.
- 88.
Price, D.E; Cooksey, G; Jehu, D; et al. The management of impotence in diabetic men by vacuum tumescence therapy. Diabet. Med. 1991, 8, 964–967. https://doi.org/10.1111/j.1464-5491.1991.tb01538.x.
- 89.
Yap, R.L; McVary, K.T; Topical agents and erectile dysfunction: Is there a place? Curr. Urol. Rep. 2002, 3, 471–476. https://doi.org/10.1007/s11934-002-0100-x.
- 90.
Porst, H. The rationale for prostaglandin E1 in erectile failure: A survey of worldwide experience. J. Urol. 1996, 155, 802–815.
- 91.
Corinaldesi, C; Di Luigi, L; Lenzi, A; et al. Phosphodiesterase type 5 inhibitors: Back and forward from cardiac indications. J. Endocrinol. Invest. 2016, 39, 143–151. https://doi.org/10.1007/s40618-015-0340-5.
- 92.
Kloner, R; Padma-Nathan, H; Erectile dysfunction in patients with coronary artery disease. Int. J. Impot. Res. 2005, 17, 209–215. https://doi.org/10.1038/sj.ijir.3901309.
- 93.
Rassweiler, J.J; Knoll, T; Köhrmann, K.U; et al. Shock wave technology and application: An update. Eur. Urol. 2011, 59, 784–796. https://doi.org/10.1016/j.eururo.2011.02.033.
- 94.
Vardi, Y; Appel, B; Jacob, G; et al. Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur. Urol. 2010, 58, 243–248. https://doi.org/10.1016/j.eururo.2010.04.004.
- 95.
Nishida, T; Shimokawa, H; Oi, K; et al. Extracorporeal cardiac shock wave therapy markedly ameliorates ischemia-induced myocardial dysfunction in pigs in vivo. Circulation 2004, 110, 3055–3061. https://doi.org/10.1161/01.Cir.0000148849.51177.97.
- 96.
Gandaglia, G; Briganti, A; Jackson, G; et al. A systematic review of the association between erectile dysfunction and cardiovascular disease. Eur. Urol. 2014, 65, 968–978. https://doi.org/10.1016/j.eururo.2013.08.023.
- 97.
Shindel, A.W; Kishore, S; Lue, T.F; Drugs designed to improve endothelial function: Effects on erectile dysfunction. Curr. Pharm. Des. 2008, 14, 3758–3767. https://doi.org/10.2174/138161208786898752.
- 98.
Klomjit, N; Lerman, A; Lerman, L.O; It Comes As a Shock: Kidney Repair Using Shockwave Therapy. Hypertension 2020, 76, 1696–1703. https://doi.org/10.1161/hypertensionaha.120.14595.
- 99.
Sundaram, S; Sellamuthu, K; Nagavelu, K; et al. Stimulation of angiogenesis using single-pulse low-pressure shock wave treatment. J. Mol. Med. 2018, 96, 1177–1187. https://doi.org/10.1007/s00109-018-1690-1.
- 100.
Cooper, B; Bachoo, P; Extracorporeal shock wave therapy for the healing and management of venous leg ulcers. Cochrane Database Syst. Rev. 2018, 6, Cd011842. https://doi.org/10.1002/14651858.CD011842.pub2.
- 101.
Canguven, O; Khalafalla, K; Al Ansari, A; Low-intensity extracorporeal shockwave therapy for erectile dysfunction. Arab J. Urol. 2021, 19, 340–345. https://doi.org/10.1080/2090598x.2021.1948158.
- 102.
Rizk, P.J; Krieger, J.R; Kohn, T.P; et al. Low-Intensity Shockwave Therapy for Erectile Dysfunction. Sex. Med. Rev. 2018, 6, 624–630. https://doi.org/10.1016/j.sxmr.2018.01.002.
- 103.
Cui, X; Zhou, J; Qin, Z; et al. Acupuncture for Erectile Dysfunction: A Systematic Review. Biomed. Res. Int. 2016, 2016, 2171923. https://doi.org/10.1155/2016/2171923.
- 104.
Cui, X; Li, X; Peng, W; et al. Acupuncture for erectile dysfunction: A systematic review protocol. BMJ Open 2015, 5, e007040. https://doi.org/10.1136/bmjopen-2014-007040.
- 105.
Zhang, H; Albersen, M; Jin, X; et al. Stem cells: Novel players in the treatment of erectile dysfunction. Asian J. Androl. 2012, 14, 145–155. https://doi.org/10.1038/aja.2011.79.
- 106.
Sun, C; Lin, H; Yu, W; et al. Neurotrophic effect of bone marrow mesenchymal stem cells for erectile dysfunction in diabetic rats. Int. J. Androl. 2012, 35, 601–607. https://doi.org/10.1111/j.1365-2605.2012.01250.x.
- 107.
Lin, G; Banie, L; Ning, H; et al. Potential of adipose-derived stem cells for treatment of erectile dysfunction. J. Sex. Med. 2009, 6, 320–327. https://doi.org/10.1111/j.1743-6109.2008.01190.x.
- 108.
Mangner, N; Linke, A; Oberbach, A; et al. Exercise training prevents TNF-α induced loss of force in the diaphragm of mice. PLoS ONE 2013, 8, e52274. https://doi.org/10.1371/journal.pone.0052274.
- 109.
Haahr, M.K; Harken Jensen, C; Toyserkani, N.M; et al. A 12-Month Follow-up After a Single Intracavernous Injection of Autologous Adipose-Derived Regenerative Cells in Patients with Erectile Dysfunction Following Radical Prostatectomy: An Open-Label Phase I Clinical Trial. Urology 2018, 121, e206. https://doi.org/10.1016/j.urology.2018.06.018.
- 110.
Yiou, R; Hamidou, L; Birebent, B; et al. Intracavernous Injections of Bone Marrow Mononucleated Cells for Postradical Prostatectomy Erectile Dysfunction: Final Results of the INSTIN Clinical Trial. Eur. Urol. Focus 2017, 3, 643–645. https://doi.org/10.1016/j.euf.2017.06.009.
- 111.
Protogerou, V; Beshari, S.E; Michalopoulos, E; et al. The Combined Use of Stem Cells and Platelet Lysate Plasma for the Treatment of Erectile Dysfunction: A Pilot Study-6 Months Results. Medicines 2020, 7, 14. https://doi.org/10.3390/medicines7030014.
- 112.
Levy, J.A; Marchand, M; Iorio, L; et al. Determining the Feasibility of Managing Erectile Dysfunction in Humans With Placental-Derived Stem Cells. J. Am. Osteopath. Assoc. 2016, 116, e1–e5. https://doi.org/10.7556/jaoa.2016.007.
- 113.
Scott, F.B; Bradley, W.E; Timm, G.W; Management of erectile impotence. Use of implantable inflatable prosthesis. Urology 1973, 2, 80–82. https://doi.org/10.1016/0090-4295(73)90224-0.
- 114.
Montorsi, F; Rigatti, P; Carmignani, G; et al. AMS three-piece inflatable implants for erectile dysfunction: A long-term multi-institutional study in 200 consecutive patients. Eur. Urol. 2000, 37, 50–55. https://doi.org/10.1159/000020099.
- 115.
Pastuszak, A.W; Lentz, A.C; Farooq, A; et al. Technological Improvements in Three-Piece Inflatable Penile Prosthesis Design over the Past 40 Years. J. Sex. Med. 2015, 12, 415–421. https://doi.org/10.1111/jsm.13004.
- 116.
Dell’Atti, L; Slyusar, V; Cambise, C; Multimodal treatments based on Tadalafil during acute phase of Peyronie’s disease: Experience at two referral academic centers. Ir. J. Med. Sci. 2024, 193, 2301–2306. https://doi.org/10.1007/s11845-024-03734-1.
- 117.
Assaly-Kaddoum, R; Giuliano, F; Laurin, M; et al. Low Intensity Extracorporeal Shock Wave Therapy Improves Erectile Function in a Model of Type II Diabetes Independently of NO/cGMP Pathway. J. Urol. 2016, 196, 950–956. https://doi.org/10.1016/j.juro.2016.03.147.
- 118.
Verze, P; Capece, M; Creta, M; et al. Efficacy and safety of low-intensity shockwave therapy plus tadalafil 5 mg once daily in men with type 2 diabetes mellitus and erectile dysfunction: A matched-pair comparison study. Asian J. Androl. 2020, 22, 379–382. https://doi.org/10.4103/aja.aja_121_19.
- 119.
Adefegha, S.A; Oboh, G; Okeke, B.M; et al. Comparative Effects of Alkaloid Extracts from Aframomum melegueta (Alligator Pepper) and Aframomum danielli (Bastered Melegueta) on Enzymes Relevant to Erectile Dysfunction. J. Diet. Suppl. 2017, 14, 542–552. https://doi.org/10.1080/19390211.2016.1272661.
- 120.
Ademiluyi, A.O; Oyeniran, O.H; Jimoh, T.O; et al. Fluted pumpkin (Telfairia occidentalis) seed modulates some markers of erectile function in isolated rat’s corpus cavernosum: Influence of polyphenol and amino acid constituents. J. Food Biochem. 2019, 43, e13037. https://doi.org/10.1111/jfbc.13037.

This work is licensed under a Creative Commons Attribution 4.0 International License.


