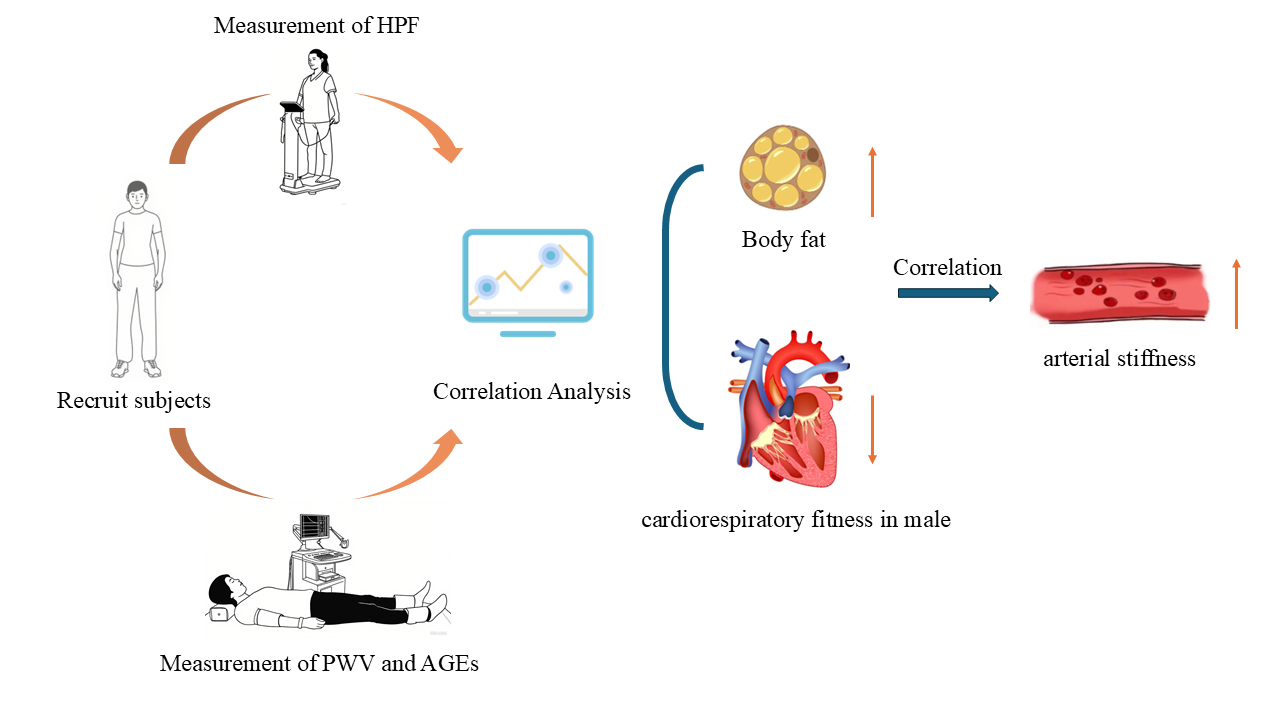
Objective: The aim of this study was to explore the relationship between health-related physical fitness (HPF) and arterial stiffness, which was evaluated using skin autofluorescence (AF) to measure advanced glycosylation end products (AGEs) and pulse wave velocity (PWV). Methods: The 132 young adults aged 20–30 were recruited for this study. According to the National Physical Fitness Standards Manual, HPF was measured by the indicators that reflect the body composition, cardiopulmonary fitness, muscular fitness and flexibility. AGEs were evaluated through AF, which performed using a non-invasive detection system. PWV was measured by Pulse wave velocity measurement system. Spearman correlation analysis and multiple linear regression analysis were used for data analysis. Results: AF in young adults, whether male or female, was positively correlated with BMI and body fat (BF) (male: p = 0.013, p = 0.0004, female: p = 0.049, p = 0.015 with BMI and BF, respectively). AF in male young adults was negatively correlated with the cardiorespiratory endurance index (CEI) (p = 0.046). Multiple linear regression adjusted for age showed that AF and BF were positively correlated for only male young adults (p = 0.032). There was no significant correlation between the carotid-femoral or carotid-radial pulse wave velocity (CFPWV or CRPWV) and AF or any of the HPF indicators in the undergraduate participants (p > 0.05). Conclusion: BMI and body fat are the main factors affecting the risk of arterial stiffness in young adults, whether male or female. In addition, cardiorespiratory fitness is also the main factor for the risk of chronic disease in young male adults. It is suggested that young male adults should pay more attention to the exercise of cardiorespiratory fitness.
- Open Access
- Article
An Observational Study on the Associations between Arterial Stiffness and Health-Related Physical Fitness in Young Adults
- Long-Long Liu,
- Jing Zhang *,
- Qian Xie,
- Yuan Zhou,
- Bo Ye,
- Wan-Wan Wang,
- Wen-Xin Wei,
- Liang-Liang Yan,
- Xiao-Long Li
Author Information
Received: 27 Apr 2025 | Revised: 03 Jun 2025 | Accepted: 12 Aug 2025 | Published: 03 Sep 2025
Abstract
Graphical Abstract
Keywords
health-related physical fitness | autofluorescence | advanced glycosylation end products | pulse wave velocity
References
- 1.Kasmauski, K. Type 2 diabetes: The urgent need to protect young people. Lancet 2018, 392, 2325. https://doi.org/10.1016/S0140-6736(18)33015-0.
- 2.Andersson, C.; Vasan, R.S. Epidemiology of cardiovascular disease in young individuals. Nat. Rev. Cardiol. 2018, 15, 230–240. https://doi.org/10.1038/nrcardio.2017.154.
- 3.Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. https://doi.org/10.1002/cphy.c110025.
- 4.Jayedi, A.; Soltani, S.; Abdolshahi, A.; Shab-Bidar, S. Healthy and unhealthy dietary patterns and the risk of chronic disease: An umbrella review of meta-analyses of prospective cohort studies. Br. J. Nutr. 2020, 124, 1133–1144. https://doi.org/10.1017/S0007114520002330.
- 5.Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child. Adolesc. Health 2020, 4, 23–35. https://doi.org/10.1016/S2352-4642(19)30323-2.
- 6.Ashton, L.M.; Hutchesson, M.J.; Rollo, M.E.; Morgan, P.J.; Collins, C.E. Motivators and Barriers to Engaging in Healthy Eating and Physical Activity. Am. J. Mens. Health 2017, 11, 330–343. https://doi.org/10.1177/1557988316680936.
- 7.Bi, J.; Huang, Y.; Xiao, Y.; Cheng, J.; Li, F.; Wang, T.; Zhao, X. Association of lifestyle factors and suboptimal health status: A cross-sectional study of Chinese students. BMJ Open 2014, 4, e005156. https://doi.org/10.1136/bmjopen-2014-005156.
- 8.Ng, R.; Sutradhar, R.; Yao, Z.; Wodchis, W.P.; Rosella, L.C. Smoking, drinking, diet and physical activity-modifiable lifestyle risk factors and their associations with age to first chronic disease. Int. J. Epidemiol. 2020, 49, 113–130. https://doi.org/10.1093/ije/dyz078.
- 9.Hodes, R.J.; Lakatta, E.G.; McNeil, C.T. Another modifiable risk factor for cardiovascular disease? Some evidence points to arterial stiffness. J. Am. Geriatr. Soc. 1995, 43, 581–582. https://doi.org/10.1111/j.1532-5415.1995.tb06111.x.
- 10.Gelžinský, J.; Mayer, O., Jr.; Seidlerová, J.; Mateřánková, M.; Mareš, Š.; Kordíkova, V.; Filipovský, J. Serum biomarkers, skin autofluorescence and other methods. Which parameter better illustrates the relationship between advanced glycation end products and arterial stiffness in the general population? Hypertens. Res. 2021, 44, 518–527. https://doi.org/10.1038/s41440-020-00601-1.
- 11.Singh, R.B.A.M.; Barden, A.; Mori, T.; Beilin, L. Advanced glycation end-products: A review. Diabetologia 2001, 44, 129–146. https://doi.org/10.1007/s001250051591.
- 12.Davis, K.E.; Prasad, C.; Vijayagopal, P.; Juma, S.; Imrhan, V. Advanced Glycation End Products, Inflammation, and Chronic Metabolic Diseases: Links in a Chain? Crit. Rev. Food Sci. Nutr. 2016, 56, 989–998. https://doi.org/10.1080/10408398.2012.744738.
- 13.Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131.
- 14.Dalal, M.; Ferrucci, L.; Sun, K.; Beck, J.; Fried, L.P.; Semba, R.D. Elevated serum advanced glycation end products and poor grip strength in older community-dwelling women. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 132–137. https://doi.org/10.1093/gerona/gln018.
- 15.Albin, E.E.; Brellenthin, A.G.; Lang, J.A.; Meyer, J.D.; Lee, D.C. Cardiorespiratory Fitness and Muscular Strength on Arterial Stiffness in Older Adults. Med. Sci. Sports Exerc. 2020, 52, 1737–1744. https://doi.org/10.1249/MSS.0000000000002319.
- 16.Jae, S.Y.; Heffernan, K.S.; Fernhall, B.; Oh, Y.S.; Park, W.H.; Lee, M.K.; Choi, Y.H. Association between cardiorespiratory fitness and arterial stiffness in men with the metabolic syndrome. Diabetes Res. Clin. Pract. 2010, 90, 326–332. https://doi.org/10.1016/j.diabres.2010.08.025.
- 17.Devesa, A.; Ibanez, B.; Malick, W.A.; Tinuoye, E.O.; Bustamante, J.; Peyra, C.; Fuster, V. Primary Prevention of Subclinical Atherosclerosis in Young Adults: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2023, 82, 2152–2162. https://doi.org/10.1016/j.jacc.2023.09.817.
- 18.Lu, Y.; Kiechl, S.J.; Wang, J. Global distributions of age- and sex-related arterial stiffness: Systematic review and meta-analysis of 167 studies with 509,743 participants. EBioMedicine 2023, 92, 104619. https://doi.org/10.1016/j.ebiom.2023.104619.
- 19.Meani, P.; Maloberti, A.; Sormani, P.; Colombo, G.; Giupponi, L.; Stucchi, M.; ; Giannattasio, C. Determinants of carotid-femoral pulse wave velocity progression in hypertensive patients over a 3.7 years follow-up. Blood Press. 2018, 27, 32–40. https://doi.org/10.1080/08037051.2017.1378069.
- 20.Ashor, A.W.; Lara, J.; Siervo, M.; Celis-Morales, C.; Mathers, J.C. Effects of exercise modalities on arterial stiffness and wave reflection: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2014, 9, e110034. https://doi.org/10.1371/journal.pone.0110034.
- 21.Chaudhuri, J.; Bains, Y.; Guha, S.; Kahn, A.; Hall, D.; Bose, N.; Kapahi, P. The role of advanced glycation end products in aging and metabolic diseases: Bridging association and causality. Cell Metab. 2018, 28, 337–352. https://doi.org/10.1016/j.cmet.2018.08.014.
- 22.Gallagher, J.R.; Brouha, L.V. A Simple Method of Evaluating Fitness in Boys: The Step Test. Yale J. Biol. Med. 1943, 15, 769–779.
- 23.Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34.
- 24.Mahali, S.K.; Verma, N.; Manna, S.K. Advanced glycation end products induce lipogenesis: Regulation by natural xanthone through inhibition of ERK and NF-κB. J. Cell Physiol. 2014, 229, 1972–1980. https://doi.org/10.1002/jcp.24647.
- 25.Den Engelsen, C.; van den Donk, M.; Gorter, K.J.; Salomé, P.L.; Rutten, G.E. Advanced glycation end products measured by skin autofluorescence in a population with central obesity. Dermatoendocrinology 2012, 4, 33–38. https://doi.org/10.4161/derm.17999.
- 26.Lutgers, H.L.; Graaff, R.; Links, T.P.; Ubink-Veltmaat, L.J.; Bilo, H.J.; Gans, R.O.; Smit, A.J. Skin autofluorescence as a noninvasive marker of vascular damage in patients with type 2 diabetes. Diabetes Care 2006, 29, 2654–2659. https://doi.org/10.2337/dc05-2173.
- 27.Köchli, S.; Endes, K.; Trinkler, M.; Mondoux, M.; Zahner, L.; Hanssen, H. Association of physical fitness with skin autofluorescence-derived advanced glycation end products in children. Pediatr. Res. 2020, 87, 1106–1111. https://doi.org/10.1038/s41390-019-0694-z.
- 28.Vianello, E.; Beltrami, A.P.; Aleksova, A.; Janjusevic, M.; Fluca, A.L.; Corsi Romanelli, M.M.; Dozio, E. The Advanced Glycation End-Products (AGE)-Receptor for AGE System (RAGE): An Inflammatory Pathway Linking Obesity and Cardiovascular Diseases. Int. J. Mol. Sci. 2025, 26, 3707. https://doi.org/10.3390/ijms26083707.
- 29.Su, X.; Looney, M.R.; Gupta, N.; Matthay, M.A. Receptor for advanced glycation end-products (RAGE) is an indicator of direct lung injury in models of experimental lung injury. Am. J. Physiol. Lung Cell Mol. Physiol. 2009, 297, L1–L5. https://doi.org/10.1152/ajplung.90546.2008.
- 30.He, M.; Kubo, H.; Ishizawa, K.; Hegab, A.E.; Yamamoto, Y.; Yamamoto, H.; Yamaya, M. The role of the receptor for advanced glycation end-products in lung fibrosis. Am. J. Physiol. Lung Cell Mol. Physiol. 2007, 293, L1427–L1436. https://doi.org/10.1152/ajplung.00075.2007.
- 31.Hjerrild, J.N.; Wobbe, A.; Stausholm, M.B.; Larsen, A.E.; Josefsen, C.O.; Malmgaard-Clausen, N.M.; Couppé; C. Effects of Long-Term Physical Activity and Diet on Skin Glycation and Achilles Tendon Structure. Nutrients 2019, 11, 1409. https://doi.org/10.3390/nu11061409.
- 32.Li, Z.-G.; Liao, B.-G. Harvard bench height reform experimental study. J. Guangzhou Sports Inst. 1995, 2, 35–37. https://doi.org/10.13830/j.cnki/g8.1995.02.008 cn44-1129.
- 33.General Administration of Sport. Chinese Adult Physical Fitness Monitoring Workbook; People’s Sports Publishing House: Beijing, China, 1997; pp. 21–22.
- 34.Waqas, K.; Chen, J.; Trajanoska, K.; Ikram, M.A.; Uitterlinden, A.G.; Rivadeneira, F.; Zillikens, M.C. Skin Autofluorescence, a Noninvasive Biomarker for Advanced Glycation End-products, Is Associated with Sarcopenia. J. Clin. Endocrinol. Metab. 2022, 107, e793–e803. https://doi.org/10.1210/clinem/dgab632.
- 35.Momma, H.; Niu, K.; Kobayashi, Y.; Guan, L.; Sato, M.; Guo, H.; Nagatomi, R. Skin advanced glycation end product accumulation and muscle strength among adult men. Eur. J. Appl. Physiol. 2011, 111, 1545–1552. https://doi.org/10.1007/s00421-010-1779-x.
- 36.Tabara, Y.; Ikezoe, T.; Yamanaka, M.; Setoh, K.; Segawa, H.; Kawaguchi, T.; Nagahama Study Group. Advanced Glycation End Product Accumulation Is Associated with Low Skeletal Muscle Mass, Weak Muscle Strength, and Reduced Bone Density: The Nagahama Study. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 1446–1453. https://doi.org/10.1093/gerona/gly233.
- 37.Bowen, T.S.; Schuler, G.; Adams, V. Skeletal muscle wasting in cachexia and sarcopenia: Molecular pathophysiology and impact of exercise training. J. Cachexia Sarcopenia Muscle 2015, 6, 197–207. https://doi.org/10.1002/jcsm.12043.
- 38.Chiu, C.Y.; Yang, R.S.; Sheu, M.L.; Chan, D.C.; Yang, T.H.; Tsai, K.S.; Liu, S.H.. Advanced glycation end-products induce skeletal muscle atrophy and dysfunction in diabetic mice via a RAGE-mediated, AMPK-down-regulated, Akt pathway. J. Pathol. 2016, 238, 470–482. https://doi.org/10.1002/path.4674.
- 39.Howard, A.C.; McNeil, A.K.; Xiong, F.; Xiong, W.C.; McNeil, P.L. A novel cellular defect in diabetes: Membrane repair failure. Diabetes 2011, 60, 3034–3043. https://doi.org/10.2337/db11-0851.
- 40.Mitchell, W.K.; Williams, J.; Atherton, P.; Larvin, M.; Lund, J.; Narici, M. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front. Physiol. 2012, 3, 260. https://doi.org/10.3389/fphys.2012.00260.
- 41.Koetsier, M.; Lutgers, H.L.; De Jonge, C.; Links, T.P.; Smit, A.J.; Graaff, R. Reference values of skin autofluorescence. Diabetes Technol. Ther. 2010, 12, 399–403. https://doi.org/10.1089/dia.2009.0113.
- 42.Vianna, C.A.; Horta, B.L.; Gonzalez, M.C.; França GV, A.; Gigante, D.P.; Barros, F.L. Association of pulse wave velocity with body fat measures at 30 y of age. Nutrition 2019, 61, 38–42. https://doi.org/10.1016/j.nut.2018.09.037.
- 43.Wildman, R.P.; Mackey, R.H.; Bostom, A.; Thompson, T.; Sutton-Tyrrell, K. Measures of obesity are associated with vascular stiffness in young and older adults. Hypertension 2003, 42, 468–473. https://doi.org/10.1161/01.HYP.0000090360.78539.CD.
- 44.Brunner, E.J.; Shipley, M.J.; Ahmadi-Abhari, S.; Tabak, A.G.; McEniery, C.M.; Wilkinson, I.B.; Kivimaki, M. Adiposity, obesity, and arterial aging: Longitudinal study of aortic stiffness in the Whitehall II cohort. Hypertension 2015, 66, 294–300. https://doi.org/10.1161/HYPERTENSIONAHA.115.05494.
- 45.Petersen, K.S.; Blanch, N.; Keogh, J.B.; Clifton, P.M. Effect of weight loss on pulse wave velocity: Systematic review and meta-analysis. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 243–252. https://doi.org/10.1161/ATVBAHA.114.304798.
- 46.Yamamoto, K.; Kawano, H.; Gando, Y.; Iemitsu, M.; Murakami, H.; Sanada, K.; Miyachi, M.. Poor trunk flexibility is associated with arterial stiffening. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H1314–H1318. https://doi.org/10.1152/ajpheart.00061.2009.
- 47.Seals, D.R.; Nagy, E.E.; Moreau, K.L. Aerobic exercise training and vascular function with ageing in healthy men and women. J. Physiol. 2019, 597, 4901–4914. https://doi.org/10.1113/JP277764.
- 48.Gando, Y.; Murakami, H.; Yamamoto, K.; Kawakami, R.; Ohno, H.; Sawada, S.S.; Miyachi, M. Greater Progression of Age-Related Aortic Stiffening in Adults with Poor Trunk Flexibility: A 5-Year Longitudinal Study. Front. Physiol. 2017, 8, 454. https://doi.org/10.3389/fphys.2017.00454.
- 49.Birukov, A.; Cuadrat, R.; Polemiti, E.; Eichelmann, F.; Schulze, M.B. Advanced glycation end-products, measured as skin autofluorescence, associate with vascular stiffness in diabetic, pre-diabetic and normoglycemic individuals: A cross-sectional study. Cardiovasc. Diabetol. 2021, 20, 110. https://doi.org/10.1186/s12933-021-01296-5.
- 50.Watfa, G.; Soulis, G.; Tartagni, E.; Kearney-Schwartz, A.; Borghi, C.L.A.U.D.I.O.; Salvi, P.; Benetos, A.. Relationship between tissue glycation measured by autofluorescence and pulse wave velocity in young and elderly non-diabetic populations. Diabetes Metab. 2012, 38, 413–419. https://doi.org/10.1016/j.diabet.2012.04.004.
- 51.Palombo, C.; Kozakova, M. Arterial stiffness, atherosclerosis and cardiovascular risk: Pathophysiologic mechanisms and emerging clinical indications. Vascul Pharmacol. 2016, 77, 1–7. https://doi.org/10.1016/j.vph.2015.11.083.
- 52.Lurbe, E.; Torro, I.; Garcia-Vicent, C.; Alvarez, J.; Fernández-Fornoso, J.A.; Redon, J. Blood pressure and obesity exert independent influences on pulse wave velocity in youth. Hypertension 2012, 60, 550–555. https://doi.org/10.1161/HYPERTENSIONAHA.112.194746.
How to Cite
Liu, L.-L.; Zhang, J.; Xie, Q.; Zhou, Y.; Ye, B.; Wang, W.-W.; Wei, W.-X.; Yan, L.-L.; Li, X.-L. An Observational Study on the Associations between Arterial Stiffness and Health-Related Physical Fitness in Young Adults. Health and Metabolism 2025, 2 (4), 7. https://doi.org/10.53941/hm.2025.100030.
RIS
BibTex
Copyright & License

Copyright (c) 2025 by the authors.
This work is licensed under a Creative Commons Attribution 4.0 International License.
Contents
References